CUF Hemorrhage Control
JTS / CoTCCC
Introduction
The first phase of Tactical Combat Casualty Care (TCCC) is Care Under Fire (CUF). Care Under Fire is the care rendered by the first responder or combatant at the scene of the injury while he/she and the casualty are still under effective hostile fire. Available medical equipment is limited to that carried by the individual or by the medical provider in his or her aid bag.
Suppression of hostile fire will minimize the risk of both new casualties and additional injuries to the existing casualties. Casualty movement or extraction may be required to get them out of the kill zone before treatment should be initiated.
Massive bleeding or uncontrolled hemorrhage is the leading cause of preventable death on the battlefield, and as a result it is the number one medical priority in the CUF phase of TCCC. Early control of severe hemorrhage is critical to survival. Injury to a major vessel can quickly lead to shock and death. Due to the hostile environment encountered during CUF, only life-threatening bleeding warrants intervention.
In this module, you will learn to recognize life-threatening bleeding and the options available to control the bleeding while you are still under hostile fire. We will discuss strategies for proper tourniquet application when you have to work quickly, and identify common mistakes made during initial tourniquet applications.
Guidelines and Key Points
Basic Management Plan for Care Under Fire
- Return fire and take cover.
- Direct or expect casualty to remain engaged as a combatant if appropriate.
- Direct casualty to move to cover and apply self-aid if able.
- Try to keep the casualty from sustaining additional wounds.
- Casualties should be extricated from burning vehicles or buildings and moved to places of relative safety. Do what is necessary to stop the burning process.
- Stop life-threatening external hemorrhage if tactically feasible:
- Direct casualty to control hemorrhage by self-aid if able.
- Use a CoTCCC-recommended limb tourniquet for hemorrhage that is anatomically amenable to tourniquet use.
- Apply the limb tourniquet over the uniform clearly proximal to the bleeding site(s). If the site of the life-threatening bleeding is not readily apparent, place the tourniquet “high and tight” (as proximal as possible) on the injured limb and move the casualty to cover.
- Airway management is generally best deferred until the Tactical Field Care phase.
- There is pulsatile or steady bleeding from the wound.
- Blood is pooling on the ground.
- The overlying clothes are soaked with blood.
- Bandages or makeshift bandages used to cover the wound are ineffective and steadily becoming soaked with blood.
- There is a traumatic amputation of an arm or leg.
- There was prior bleeding, and the patient is now in shock (unconscious, confused, pale).
Tighten the tourniquet until bleeding is controlled. If the first tourniquet fails to control the bleeding, apply a second tourniquet just above the first. Don’t put a tourniquet directly over the knee or elbow. Don’t put a tourniquet directly over a holster or a cargo pocket that contains bulky items.
- Not using one when you should, or waiting too long to put it on.
- Not pulling all the slack out before tightening.
- Using a tourniquet for minimal bleeding.
- Putting it on too proximally if the bleeding site is clearly visible.
- Not taking it off when indicated during TFC.
- Taking it off when the casualty is in shock or has only a short transport time to the hospital.
- Not making it tight enough – the tourniquet should both stop the bleeding AND eliminate the distal pulse.
- Not using a second tourniquet if needed.
- Periodically loosening the tourniquet to allow blood flow to the injured extremity.
Summary
Emergency Tourniquet Use - Survival
Survival With Emergency Tourniquet Use to Stop Bleeding in Major Limb Trauma
COL John F. Kragh, Jr., MC, USA, Thomas J. Walters, PhD, David G. Baer, PhD, LTC Charles J. Fox, MC, USA, Charles E. Wade, PhD, Jose Salinas, PhD, and COL John B. Holcomb, MC, USA
Annals of Surgery
Volume 249, Number 1, January 2009
The purpose of this study at a combat support hospital in Baghdad was to determine if emergency tourniquet use saved lives.
- Tourniquets are saving lives on the battlefield.
- Improved survival when tourniquets were applied BEFORE casualties went into shock.
- 31 lives saved in this study by applying tourniquets prehospital rather than in the ED.
- In 5 casualties where a tourniquet was indicated but not used, there was a survival rate of 0% versus 87% for those casualties with tourniquet applications.
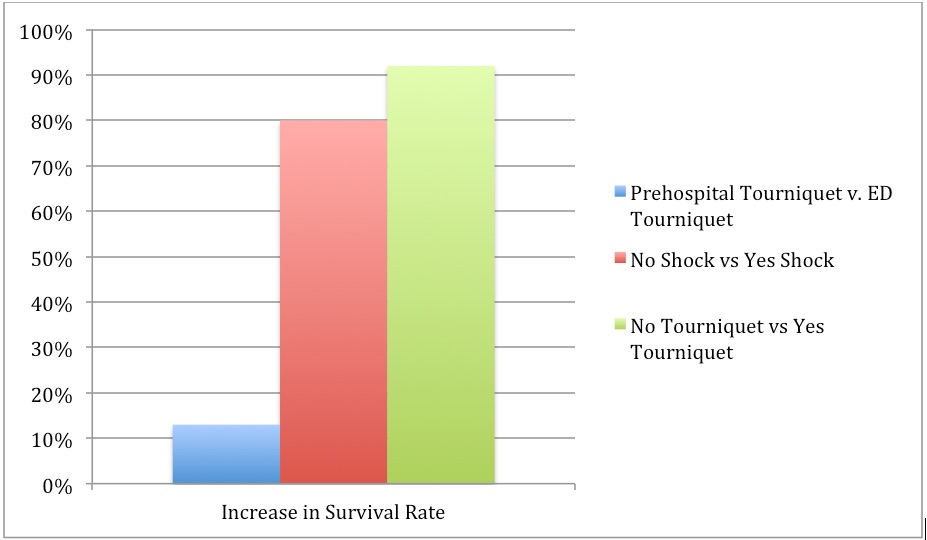
Increase in survival rate by tourniquet use. By breaking down, the tourniquet use by whether the patient was prehospital or ED, whether there was shock present or absent at the time of application, and whether tourniquets were used or not, a comparison of raw differences in survival rates indicates that the survival benefit to tourniquet use is more strongly related to tourniquet use before the patient has progressed to shock than to prehospital use.
Take Home Message:
Emergency Tourniquets - Practical Uses
Practical Use of Emergency Tourniquets to Stop Bleeding in Major Limb Trauma
John F. Kragh, Jr., MD, Thomas J. Walters, PhD, David G. Baer, PhD, Charles J. Fox, MD, Charles E. Wade, PhD, Jose Salinas, PhD, and COL John B. Holcomb, MC
The Journal of TRAUMA, Injury, Infection, and Critical Care
J Trauma. 2008;64:S38 –S50
Few studies describe the actual morbidity associated with tourniquet use in combat casualties. The purpose of this study was to measure tourniquet use and subsequent complications. A prospective survey of casualties who required tourniquets was performed at a combat support hospital in Baghdad during 7 months in 2006. Patients were evaluated for tourniquet use, limb outcome, and morbidity.
- 232 patients with tourniquets on 309 limbs
- CAT was the best field tourniquet
- Approximately 3% had transient nerve palsies
- NO amputations caused by tourniquet use
Studies on the Efficacy of Hemostatic Agents
Hemorrhage Control Studies:
Management of External Hemorrhage in Tactical Combat Casualty Care: The Adjunctive Use of XStat™ Compressed Hemostatic Sponges. TCCC Guidelines: Change 15-03.
Kyle Sims; F. Bowling, Harold Montgomery, Paul Dituro; Bijan S. Kheirabadi, PhD, Frank Butler, MD
Journal of Special Operations Medicine
J Spec Oper Med. 2016 Spring;16(1):19-28
Management of External Hemorrhage in Tactical Combat Casualty Care: Chitosan-Based Hemostatic Gauze Dressings. TCCC Guidelines – Change 13-05.
Brad L. Bennett, PhD, NREMT-P; Lanny F. Littlejohn, MD; Bijan S. Kheirabadi, PhD;
Frank K. Butler, MD; Russ S. Kotwal, MD; Michael A. Dubick, PhD; Jeffrey A. Bailey, MD
Journal of Special Operations Medicine
J Spec Oper Med. 2014 Fall;14(3):40-57
Comparison of novel hemostatic gauzes to QuikClot Combat Gauze in a standardized swine model of uncontrolled hemorrhage.
Jason M. Rall, PhD, Jennifer M. Cox, BS, Adam G. Songer, MD, Ramon F. Cestero, MD,
and James D. Ross, PhD
Journal of Trauma Acute Care Surgery
J Trauma Acute Care Surg. 2013; 75(2 Suppl 2):S150-6.
Hemostasis in a noncompressible hemorrhage model: An end-user evaluation of hemostatic agents in a proximal arterial injury.
Steven Satterly, MD, Daniel Nelson, DO, Nathan Zwintscher, MD, Morohunranti Oguntoye, MD, Wayne Causey, MD, Bryan Theis, BS, Raywin Huang, PhD, Mohamad Haque, MD,
Matthew Martin, MD, J Gerald Bickett EMT, and Robert M. Rush Jr, MD
Journal of Surgical Education
J Surg Educ. 2013;70(2):206-11.
Advanced hemostatic dressings are not superior to gauze for care under fire scenarios.
Jennifer M. Watters, MD, Philbert Y. Van, MD, Gregory J. Hamilton, BS, Chitra Sambasivan, MD, Jerome A. Differding, MPH, and Martin A. Schreiber, MD
Journal of TRAUMA Injury, Infection, and Critical Care
J Trauma 2011;70:1413-18.
Comparison of two packable hemostatic Gauze dressings in a porcine hemorrhage model.
Richard Bruce Schwartz MD, Bradford Zahner Reynolds MD, Stephen A. Shiver MD, E. Brooke Lerner PhD, Eric Mark Greenfield DO, Ricaurte A. Solis DO, Nicholas A. Kimpel DO, Phillip L. Coule MD & John G. McManus MD
Prehospital Emergency Care
Prehosp Emerg Care 2011;15:477-482
A synthesis of studies performed to evaluate the efficacy of the various hemostatic agents available at the point of injury show that they all perform equally.
Novel hemostatic devices (QuikClot Combat Gauze, QuikClot Combat Gauze XL, Celox Trauma Gauze, Celox Gauze, or HemCon ChitoGauze) perform at least as well as the current Committee on Tactical Combat Casualty Care standard for point-of-injury hemorrhage control. Despite their different compositions and sizes, the lack of clear superiority of any agent suggests that contemporary hemostatic dressing technology has potentially reached a plateau for efficacy.
There is no significant difference in hemostasis between hemostatic bandages for proximal arterial hemorrhage. Hemostasis significantly improves between 2 and 4 minutes using direct pressure and hemostatic agents. Prior medical training leads to 20% greater efficacy when using hemostatic dressings.
ChitoGauze and CombatGauze appear to be equally efficacious in their hemostatic properties, as demonstrated in a porcine hemorrhage model.
XStat (a non-absorbable, expandable, hemostatic sponge) is a new product recently approved by the FDA as a hemostatic adjunct to aid in the control of bleeding from junctional wounds in the groin or axilla. XStat is a new option for the control of external hemorrhage from junctional bleeding sites that are not adequately addressed by tourniquets, Combat gauze, Celox gauze, Chitogauze, Combat Ready Clamp, Junctional Emergency Treatment Tool, or the SAM Junctional Tourniquet.