Module 14: Eye Injuries
Joint Trauma System
Eye Injuries
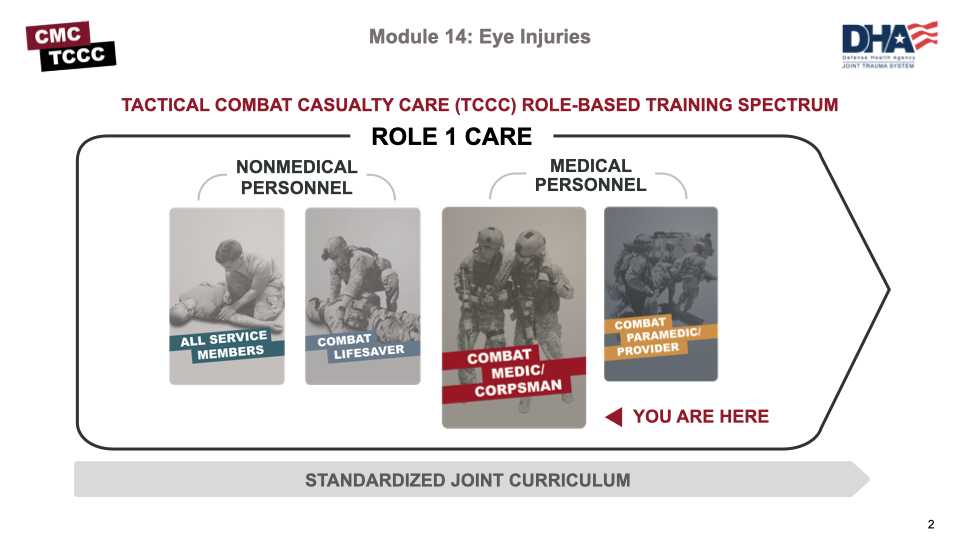
As a combat medic/corpsman, the first medical provider to care for the casualty and initiate more advanced treatments in the continuum of prehospital care, it is important that you understand the roles and responsibilities of the nonmedical personnel (All Service Members (ASM) and Combat Lifesaver (CLS)) who may be assessing casualties and providing care/assisting in the assessment and treatment of casualties with eye injuries in the prehospital environment.
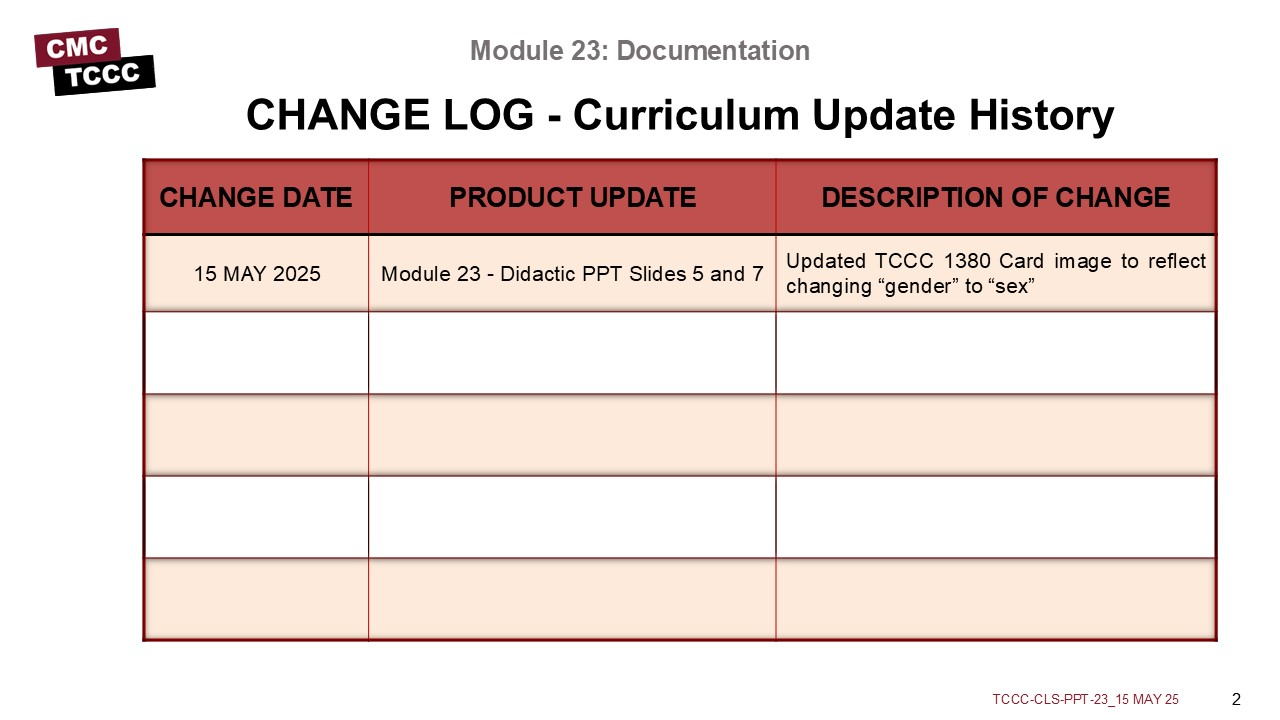
The Curriculum Change Log serves as a centralized reference to quickly track recent updates to training materials. It supports trainers by promoting clear communication, accountability, and alignment, helping stakeholders and learners understand what changes were made, why they were implemented, and when they occurred.
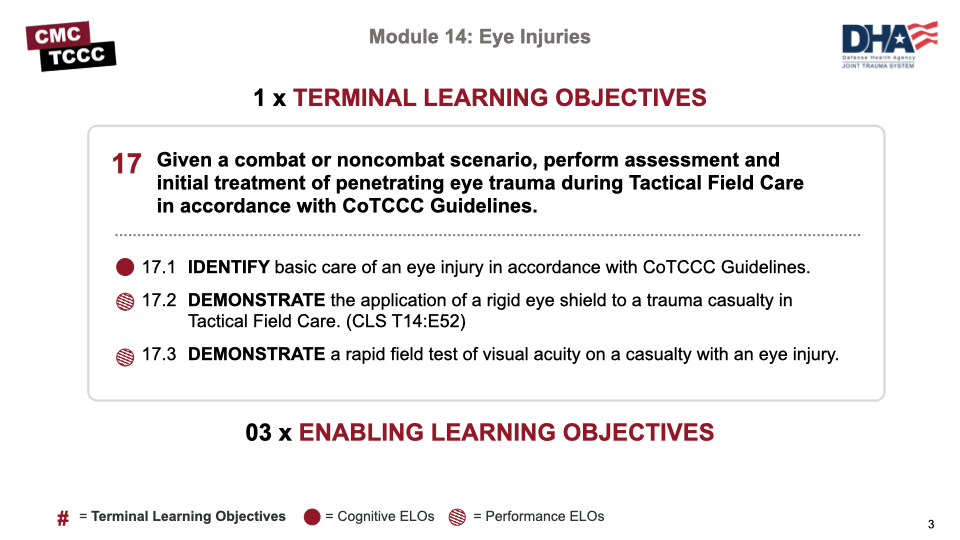
There is 1 cognitive learning objective and 2 performance learning objectives for the Eye Injuries module.
The cognitive learning objective is to identify the basic care of an eye injury in accordance with CoTCCC Guidelines.
The performance learning objectives are to demonstrate a rapid field test of visual acuity and demonstrate the application of a rigid eye shield on a trauma casualty with an eye injury.
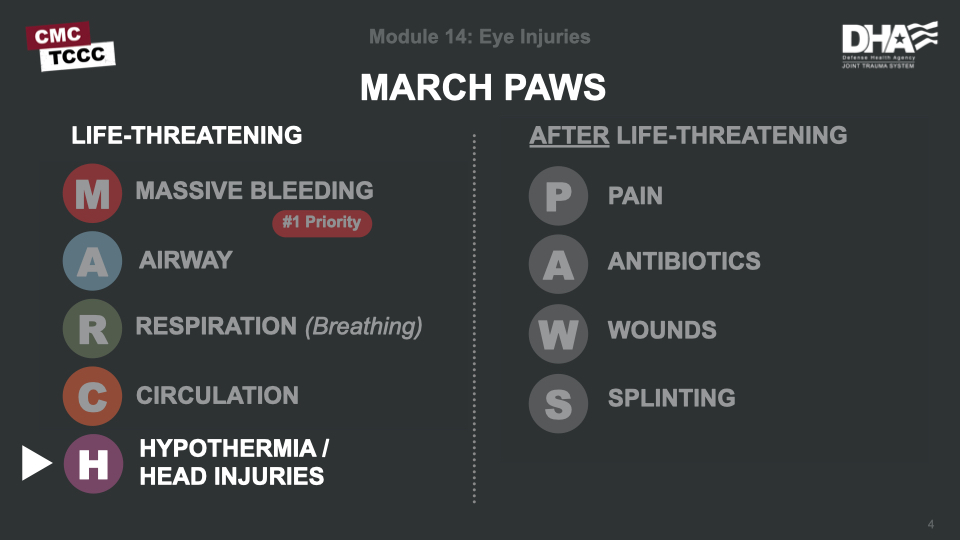
Assessment and management of eye injuries is part of the “H” in the MARCH PAWS sequence (included with head injuries).
Remember, you are now in Tactical Field Care which affords the relative safety and time to expand the focus of assessment and management beyond immediate life-threatening hemorrhage control to treatment of other injuries and prevention of potential complications including the treatment of eye injuries.
This video provides an overview of traumatic eye injuries. These injuries can occur both in training and combat operations and can lead to significant vision loss and blindness if not identified and treated in the prehospital environment. Eye injuries should be evaluated after other life-threatening injuries have been addressed.
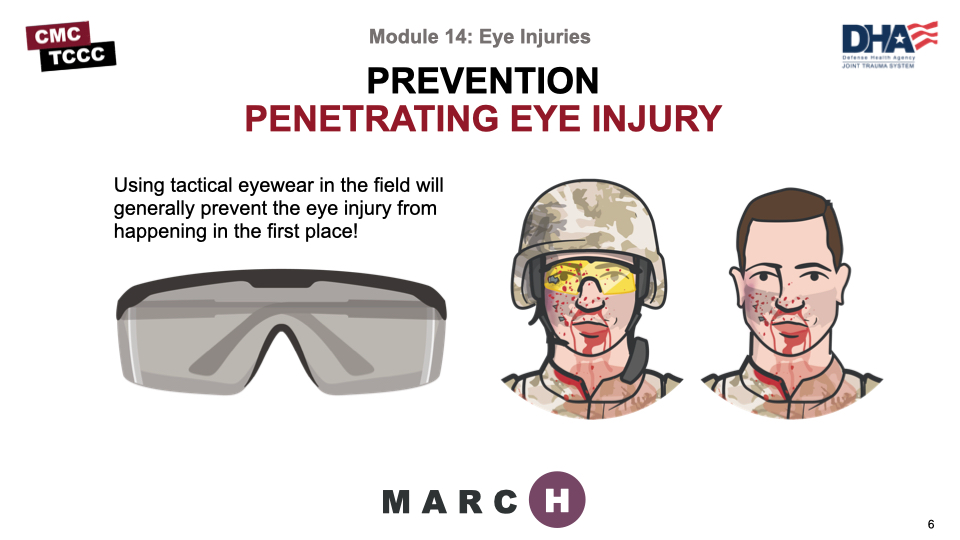
It is important to remember that most eye injuries are preventable by wearing unit-issued protective eyewear. Approved protective eyewear is very effective in stopping most metal fragments and other foreign bodies from explosions, etc. that cause the majority of eye injuries.
EYE INJURIES OVERVIEW
Vision is one of our most important senses. Damage to an eye from trauma can be irreversible and lead to permanent loss of vision or blindness if not identified and treated appropriately and as early as possible.
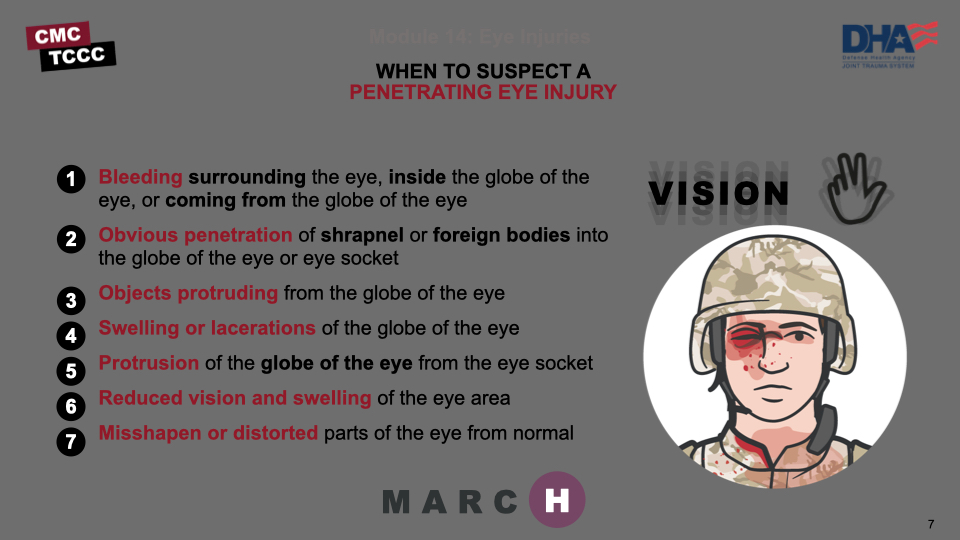
The following signs should make you suspect an eye injury:
- Bleeding surrounding the eye, inside the globe of the eye, or coming from the globe of the eye
- Obvious penetration of shrapnel or other foreign bodies into the globe of the eye or surrounding eye socket
- Objects protruding from the globe of the eye
- Swelling or lacerations of the globe of the eye
- Protrusion of the globe of the eye from the eye socket
- Reduced vision and swelling of the eye area
- Misshapen or distorted parts of the eye from normal
If a penetrating eye injury is noted or suspected, three steps must be taken:
- Perform a rapid field test of visual acuity and document findings.
- Rapid visual acuity testing includes the ability to read print, count fingers, identity hand motion, and/or differentiate light from dark.
- Cover the affected eye with a rigid eye shield, NOT a pressure patch.
- A pressure dressing could result in permanent loss of vision. Place a rigid eye shield on only one eye, unless both eyes are injured. Covering both eyes turns an otherwise ambulatory casualty into a litter casualty. Tactical eyewear is a good way to prevent eye injuries and can also be used for covering an injured eye if no eye shield is available.
- Administer the casualty’s complete Combat Wound Medication Pack (CWMP), including all the medications contained in it.
- One of the medications is 400 mg of moxifloxacin, which is administered for eye injuries to prevent infection. IV/IM antibiotics should be administered if oral moxifloxacin cannot be taken by the casualty. Penetrating eye trauma may not always be obvious injuries from bullets or shrapnel. A cut or laceration of the eye can be subtle and have the same effect allowing contents to leak from the eye. If left untreated, even apparently minor eye injuries can become infected and cause loss of vision or even blindness.
Remember: Document all findings (including visual acuity) and treatments on the casualty’s DD Form 1380
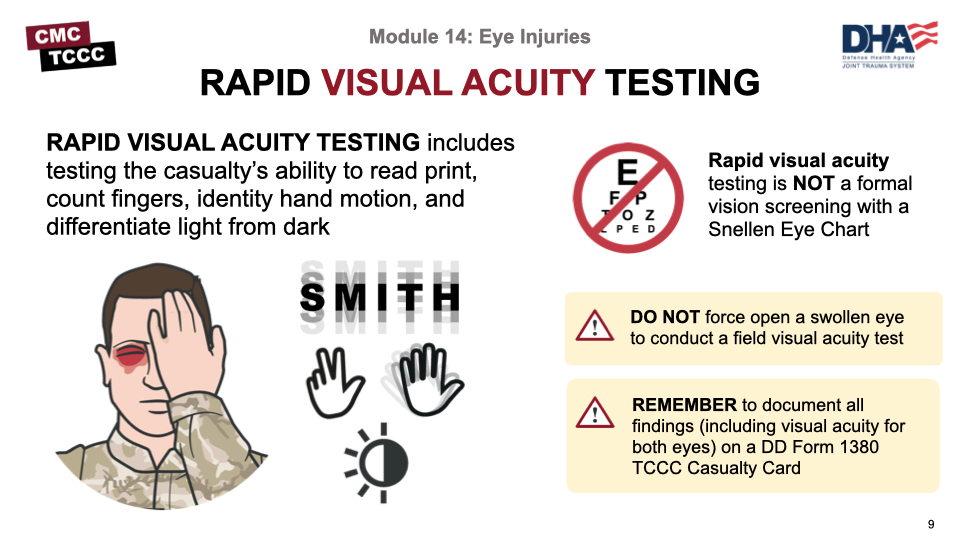
Rapid visual acuity testing is NOT a formal vision screening with a Snellen Eye Chart. It is a rapid assessment and includes testing the casualty’s ability to read print, count fingers, identity hand motion, or differentiate light from dark.
Have the casualty cover the unaffected eye. Do not force open a swollen eye to conduct a field visual acuity test.
At an arm’s length, assess the casualty’s ability to:
- Read something with text on it (that you hold up).
- If unable to read print, ask the casualty to count fingers.
- If unable to count fingers, ask the casualty to identify hand motion (by waving hand in front of affected eye).
- If unable to identify hand motion, ask the casualty to differentiate light from dark (by covering and then uncovering the affected eye).
- Repeat the procedure for the other eye.
- Determine visual acuity based on what the casualty can see (i.e., can count fingers at 2 feet).
Remember to document all findings (including visual acuity for both eyes) and treatments on a DD Form 1380 TCCC Casualty Card and attach it to the casualty.
This video demonstrates how to perform rapid field visual acuity testing on a casualty with a suspected traumatic eye injury. Note that this assessment can be performed quickly and easily.
The results should be documented on the casualty’s DD Form 1380.
PERFORMING A RAPID FIELD VISUAL ACUITY TEST
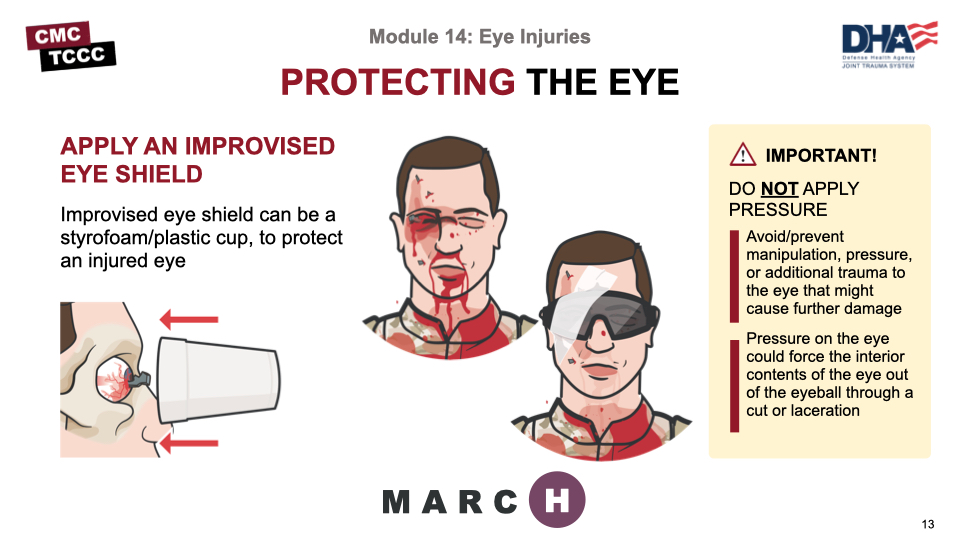
When eye trauma is suspected, it is critically important to prevent manipulation or additional trauma that might cause further damage to the eye. This can be accomplished by using a rigid shield to cover and protect the injured eye.
It is important that you do NOT apply pressure to the eye. Pressure could force the interior contents of the eye to come out of the eyeball. Pressure dressings are NOT part of the care of a traumatic eye injury and may result in permanent loss of vision.
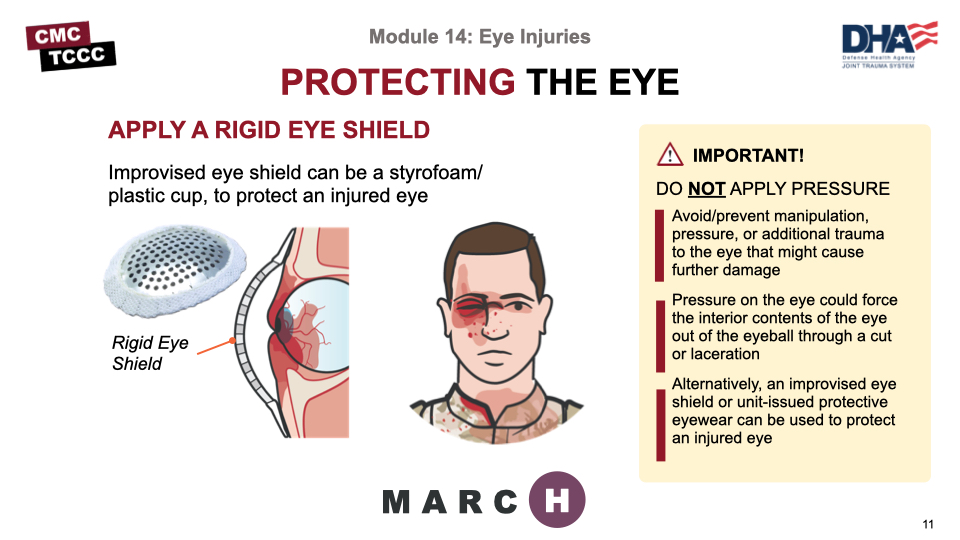
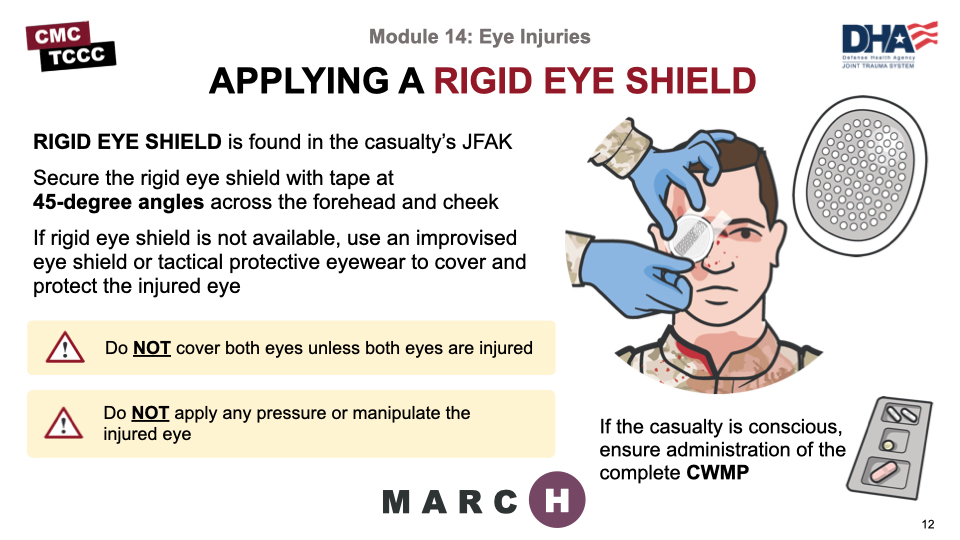
A commercially-available rigid eye shield can be found in the casualty’s JFAK and most medical kits.
Secure the rigid eye shield over the eye with tape at 45-degree angles across the forehead and cheek. For protruding or impaled objects extending past the eye shield, cut a hole in the eye shield to allow the object to fit through and secure it in place. If the eye shield cannot be applied around the impaled object, use an improvised eye shield (Styrofoam or paper cup, etc.) to protect and avoid pressure or further damage to the injured eye.
DO NOT ATTEMPT TO REMOVE.
Rigid eye shields should be placed over both eyes ONLY when you are sure or at least strongly suspect that both eyes have been injured. When only one eye has been injured, do not place an eye shield over the unaffected eye to prevent eye movement. Movement has not been shown to worsen the outcome for the injured eye. Blindness, resulting from placing eye shields over both eyes unnecessarily, is psychologically stressful and makes an otherwise ambulatory casualty a litter casualty.
Unit-issued protective eye wear can be used to protect the injured eye from further trauma, manipulation, or pressure if no other eye shield is available.
If the casualty is conscious, administer the Combat Wound Medication pack (CWMP) including the antibiotic tablet (400 mg of moxifloxacin). If unable to take the oral antibiotic in the CWMP, then administer intravenous or intramuscular antibiotics (see Antibiotic Administration Instructions covered in a later module).
Remember, if left untreated, even apparently minor eye injuries can become infected and cause loss of vision or even blindness.
When eye trauma is suspected, it is critically important to prevent manipulation or additional trauma that might cause further damage to the eye. This can be accomplished by using a rigid shield to cover and protect the injured eye. It is important that you do NOT apply pressure to the eye. Pressure could force the interior contents of the eye to come out of the eyeball. Pressure dressings are NOT part of the care of a traumatic eye injury and may result in permanent loss of vision.
Document all assessments and treatments on the casualty’s DD Form 1380 and attach it to the casualty. Be sure to include the visual acuity and any medications administered with the time administered.
This video demonstrates the proper application of a rigid eye shield on a casualty with suspected traumatic eye injury. Note that care is taken to avoid further manipulation of the eye and to avoid applying any pressure to the eye while treating the casualty.
APPLYING THE RIGID EYE SHIELD
If a penetrating eye injury is noted or suspected:
Perform a rapid field test of visual acuity and document findings.
- Rapid visual acuity testing includes the ability to read print, count fingers, identity hand motion, and/or differentiate light from dark.
Cover the affected eye with a rigid eye shield, NOT a pressure patch
- A pressure dressing could result in permanent loss of vision.
- Place a rigid eye shield on only one eye, unless both eyes are injured. Covering both eyes turns an otherwise ambulatory casualty into a litter casualty.
- Tactical eyewear is a good way to prevent eye injuries and can also be used for covering an injured eye if no eye shield is available.
Administer the casualty’s complete Combat Wound Medication Pack (CWMP), including all the medications contained in it.
- One of the medications is 400 mg of moxifloxacin, which is administered for eye injuries to prevent infection.
- IV/IM antibiotics should be administered if oral moxifloxacin cannot be taken by the casualty.
- Penetrating eye trauma may not always be obvious injuries from bullets or shrapnel. A cut or laceration of the eye can be subtle and have the same effect allowing contents to leak from the eye. If left untreated, even apparently minor eye injuries can become infected and cause loss of vision or even blindness.
Remember: Document all findings (including visual acuity) and treatments on the casualty’s DD Form 1380.
To close out this module, check your learning with the questions below (answers under the image).
Answers
What kind of dressing should be used on penetrating eye trauma with an impaled object?
A rigid eye shield should be used to cover and protect the injured eye. Alternatively, an improvised eye shield (Styrofoam or other cup, etc.) taped over the eye can be used if there is a protruding foreign body in the eye that would extend beyond the rigid eye shield. Tactical protective eyewear can be used to protect the injured eye. A pressure dressing or patch should NOT be used.
When should a pressure dressing be used in treating traumatic eye injuries?
A pressure dressing or patch should NEVER be used to treat a traumatic eye injury.
True or False: The Snellen Eye Chart is used for performing a rapid field visual acuity test?
False. Rapid visual acuity testing is NOT a formal vision screening with a Snellen Eye Chart. It is a rapid assessment and includes testing the casualty’s ability to read print, count fingers, identify hand motion, or differentiate light from dark.
True or False: Only the injured eye should be covered with a rigid eye shield?
True. Rigid eye shields should be placed over both eyes ONLY when you are sure or at least strongly suspect that both eyes have been injured. When only one eye has been injured, do not place an eye shield over the unaffected eye to prevent eye movement. Movement has not been shown to worsen the outcome for the injured eye. Blindness, resulting from placing eye shields over both eyes unnecessarily, is psychologically stressful and makes an otherwise ambulatory casualty a litter casualty.