K9 Clinical Practice Guideline #16- Analgesia and Anesthesia
K9 Combat Casualty Care Committee
Introduction
- These clinical practice guidelines (CPGs) apply to deployed human healthcare providers (HCPs) in combat or austere areas of operations. Veterinary care is established at multiple locations throughout theater, and the veterinary health care team is the MWD’s primary provider. However, HCPs are often the only medical personnel available to MWDs that are critically ill or injured. The reality is that HCPs will routinely manage working dogs in emergencies before they are ever seen by veterinary personnel.
- Care by HCPs is limited to circumstances in which the dog is too unstable to transport to supporting veterinary facilities or medical evacuation is not possible due to weather or mission constraints; immediate care is necessary to preserve life, limb, or eyesight; and veterinary personnel are not available. HCPs should only perform medical or surgical procedures – within the scope of their training or experience – necessary to manage problems that immediately threaten life, limb, or eyesight, and to prepare the dog for evacuation to definitive veterinary care. Routine medical, dental, or surgical care is not to be provided by HCPs.
- Emergent surgical management of injured MWDs may be necessary by HCPs to afford a chance at patient survival. This should be considered only if:
- The provider has the necessary advanced surgical training and experience.
- The provider feels there is a reasonable likelihood of success.
- The provider has the necessary support staff, facilities, and monitoring and intensive care facilities to manage the post-operative MWD without compromising human patient care.
- Emergent surgical management should be considered only in Role 2 or higher medical facilities and by trained surgical specialists with adequate staff. Direct communication with a US military veterinarian is essential before considering surgical management, and during and after surgery, to optimize outcome.
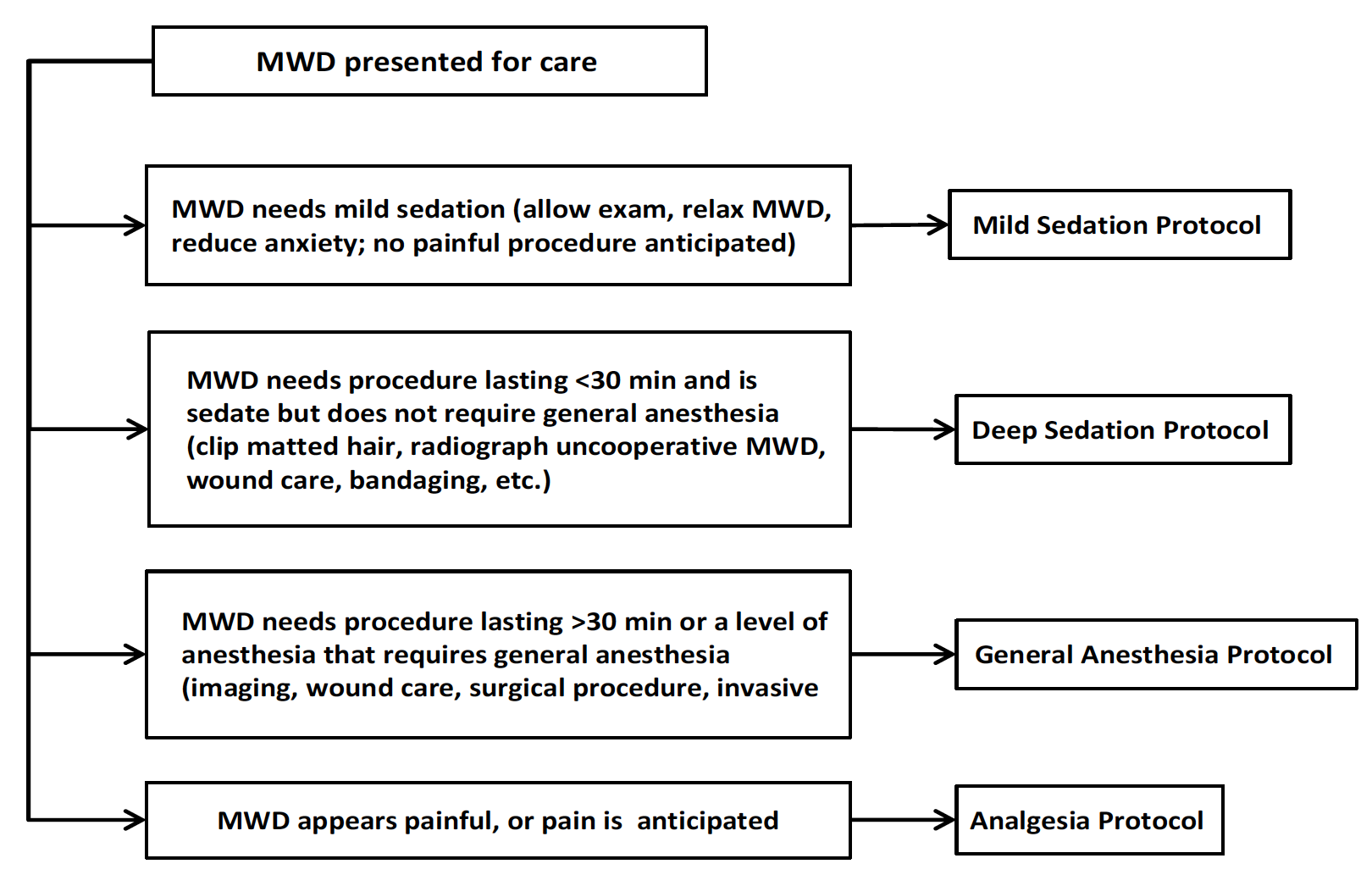
This CPG provides succinct, quick reference protocols for analgesia and anesthesia of emergently ill or injured MWDs, using simple combinations of drugs readily available to most HCPs.1 A decision-making algorithm is provided below (Figure 45) to determine which analgesia or anesthesia protocol is recommended, based on specific need. Before any use of analgesia or anesthesia, a full physical exam must be performed.
MWDs can be fractious and difficult to manage, and often require heavy sedation for relatively simple procedures. Tailored protocols are provided, based on the level of sedation or anesthesia required – mild or deep sedation, or general anesthesia.1
Figure 45. Decision-Making Algorithm for Analgesia or Anesthesia
Prehospital Analgesia
MWD handlers or combat medics may have given morphine, fentanyl, or ketamine before arrival, so inquire about drug use before transport, which may affect assessment of the patient’s mentation and analgesia.
Protocol Guidance
All drug combinations use the intramuscular (IM) route for ease and safety. If used within 5 minutes, all drugs can be combined in the same syringe to simplify administration. Wait at least 20 minutes after administration before attempting any procedure, to allow maximal drug effect. Ideally, an IV catheter should be placed once feasible (See CPG 2).
Drug Dosing in Dogs
Dosages for many analgesics in dogs are significantly higher than for people. Trust the doses provided in this CPG, and dose as directed to prevent inadequate analgesia or sedation and ‘wind up’ pain.
Gastrointestinal Side Effects of Opioids
Protocols include opioids, which in dogs typically causes emesis, often within 5 minutes of administration. Use caution and have the handler prepared to remove the muzzle to minimize aspiration risk.
Mild Sedation Protocol
- Use to relax MWDs for examination, handling, or short minor procedures that will not cause pain. Use to reduce anxiety.
- Protocol: MIDAZOLAM 0.3 mg/kg IM and HYDROMORPHONE 0.2 mg/kg IM.
- Expectations: The MWD will be calm, but reactive and noise sensitive.
Deep Sedation Protocol
- Use for procedures that can be completed in <30 minutes and do not require general anesthesia, such as clipping of hair, wound cleansing, minor wound debridement, splinting of lower limb fractures, bandage application or removal, ear cleaning, or radiography. First-line protocol for fractious MWDs.
- Protocol: MIDAZOLAM 0.3 mg/kg IM and KETAMINE 5 mg/kg IM and HYDROMORPHONE 0.1 mg/kg IM.
- If deeper sedation or light anesthesia is necessary, or to allow general anesthesia induction, use PROPOFOL in 1 mg/kg boluses IV as needed.
- Expectations: The MWD will not be able to walk, cannot be intubated, can be aroused with stimulation, and maintains laryngeal and palpebral reflexes.
General Anesthesia Protocol
- Use to facilitate imaging, allow management of fractures, perform surgical procedures, and perform invasive diagnostic procedures.
- Preoxygenate for 5 minutes using oxygen mask.
- Premedicate using the Deep Sedation Protocol, and place an IV catheter.
- Induce using PROPOFOL 1 mg/kg IV boluses to effect.
- Intubate with an appropriate endotracheal tube.
- Most MWDs require a 9-11 mm ID endotracheal tube. Use a cuffed tube.
- Maintain anesthesia using:
- ISOFLURANE 0.5-1.5% titrated to effect in 100% oxygen or
- SEVOFLURANE 2.0-2.5% titrated to effect in 100% oxygen or
- PROPOFOL CRI 100-300 mcg/kg/min.
- Manage pain with HYDROMORPHONE 0.1 mg/kg IV boluses, not to exceed 0.2 mg/kg per hour.
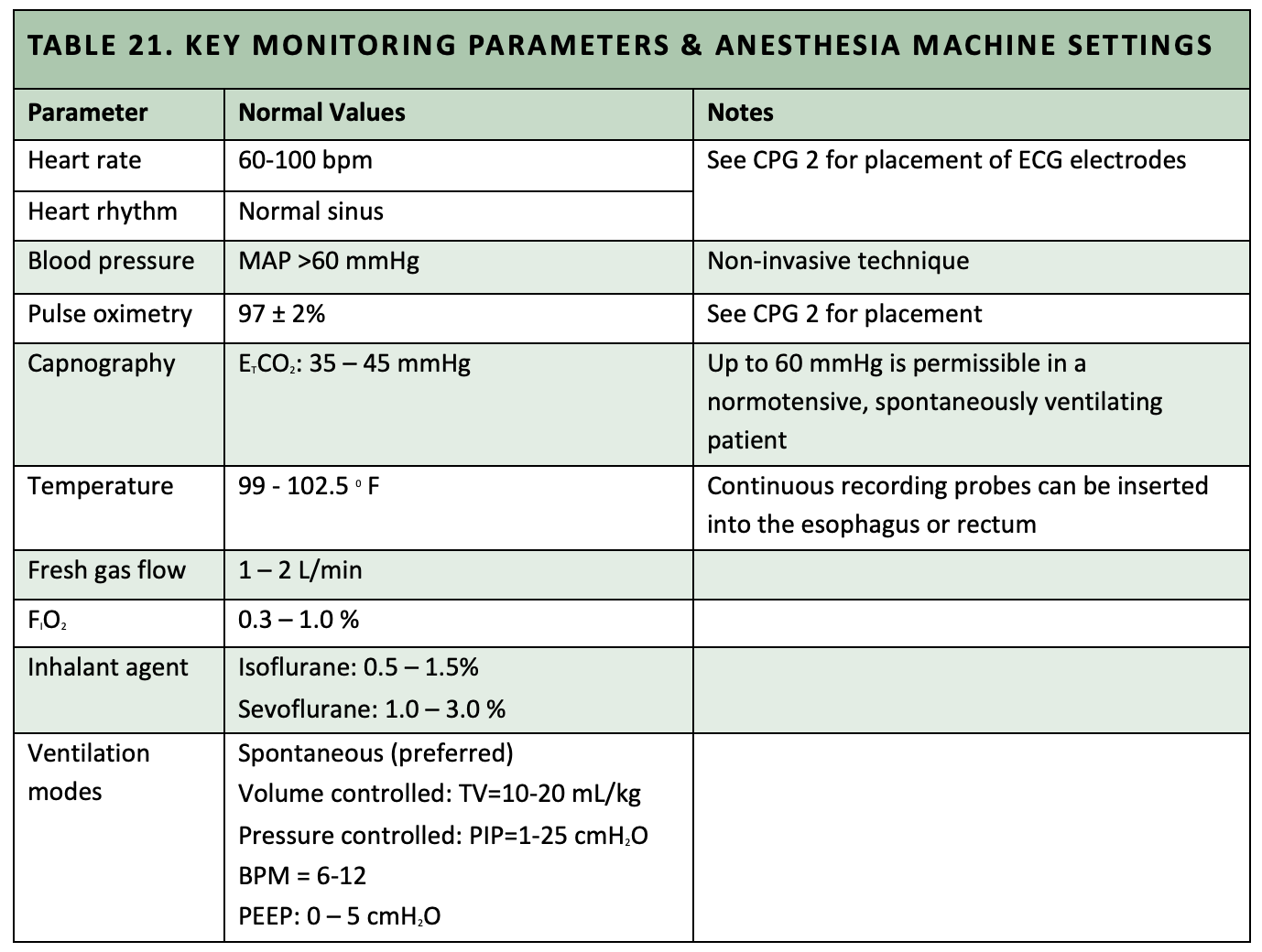
- Monitor appropriately, give IV fluids, and keep the MWD warm (See Ancillary Support in this CPG, and Table 21).
Effective Analgesia Protocols for MWDs
Assessment of pain in dogs is difficult. Dogs are generally very stoic and often hide or fail to show outward signs of pain. HCPs should err on side of providing analgesia – if performed properly, it is safe and effective, and analgesia is critically important for safe handling and alleviation of pain.
- Note that all protocols have analgesia incorporated into them. Additional analgesia can be provided by the IV, IM, or PO route, as necessary.
- Scheduled administration of analgesics in the post-procedure period is preferred to as needed administration in dogs, because pain can be difficult to assess and to avert the ‘roller coaster‘ effect of unmanaged pain.
- For intermittent IV or IM supplementary analgesia, use one of the following drugs:
- HYDROMORPHONE 0.1-0.2 mg/kg q2-4h.
- MORPHINE 0.2-0.5 mg/kg q4-6h
- For CRI supplementary analgesia, use one of the following drugs:
- FENTANYL 2-10 mcg/kg/h.
- MORPHINE 0.1-0.25 mg/kg/h.
- HYDROMORPHONE 0.02-0.05 mg/kg/h.
- For PO supplementary analgesia, use TRAMADOL 5-10 mg/kg PO q8-12h for up to 5 days.
Caution: Do NOT use acetaminophen or ibuprofen in MWDs, as these drugs can cause liver toxicity. AVOID use of NSAIDs such as naproxen, meloxicam, and aspirin in emergently ill or injured MWDs.
Opioid Reversal
At appropriate doses, dogs appear less susceptible to opioid-induced respiratory depression and excessive sedation. However, opioid side effects can be reversed in the dog using NALOXONE 0.01-0.02 mg/kg slow IV to effect if needed. Note that this will reverse analgesia as well as sedation!
Ancillary Support
- Any MWD that is deeply sedated or under general anesthesia should be given IV crystalloid fluid therapy at 10 mL/kg/h to offset anesthesia-induced hypotension. Additional fluid volumes may be necessary based on the underlying problem (e.g., shock should be given IV fluids to targeted endpoints, as per CPG 6, Figure 33).
- Active warming should be provided for any MWD that is deeply sedated or under general anesthesia. Use forced-air warmers, warm water circulating blankets, heat-retaining covers, and warming tables to target a body temperature of 100-101° F. Monitor temperature post-procedure until sustained >1000 F.
- Basic and advanced monitoring of the MWD at a level considered appropriate for a human patient for the respective level of analgesia or anesthesia must be provided. Table 21 lists key monitoring parameters and goals for anesthetized MWDs, and common anesthesia machine settings.
Table 21. Key Monitoring Parameters & Anesthesia Machine Settings
References
US Army Public Health Command, Veterinary Medical Standardization Board, Anesthesia and Pain Management Standards, 10 October 2013.