Module 1: Principles and Application of Tactical Combat Casualty Care (TCCC)
Joint Trauma System
Principles and Application of Tactical Combat Casualty Care (TCCC)
Recognizing that Tactical Combat Casualty Care (TCCC) is the standard of care in battlefield prehospital medicine, DoDI 1322.24, Medical Readiness Training, implemented standardized combat casualty care training for all Service members. Training focuses on lifesaving skills and is tailored to the level of care that an individual might be expected to perform. If you have not been trained in TCCC, then your previous medical training may not have contained the material presented in the following lessons.
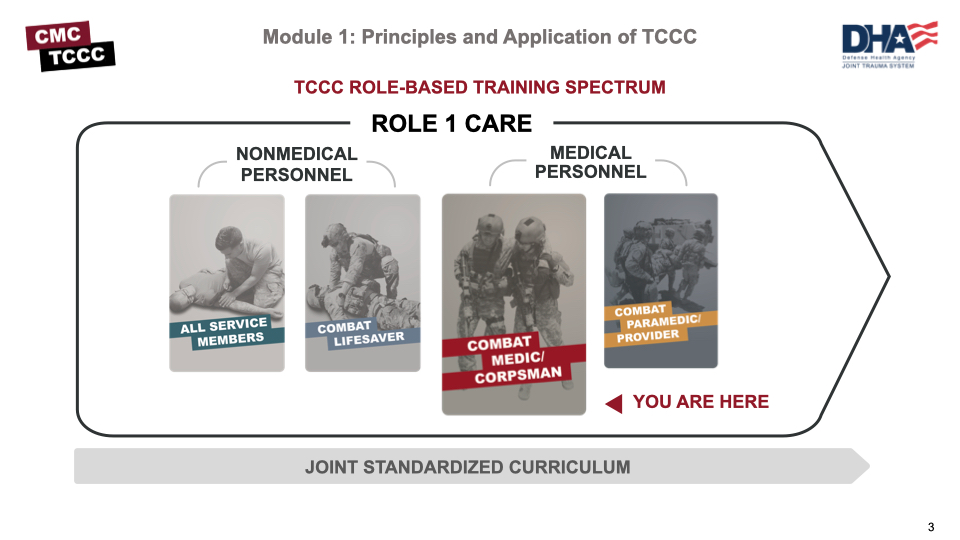
Tactical Combat Casualty Care is broken up into 4 roles of care:
- The most basic that is taught is All Service Members (ASM) and includes the absolute basics of hemorrhage control and basic recognition of more serious problems.
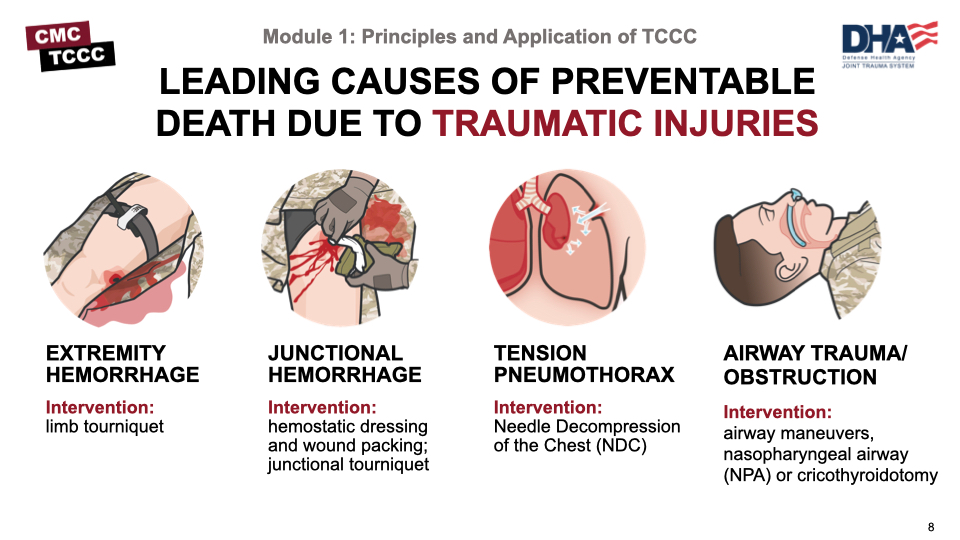
- The Combat Lifesaver (CLS) is taught more advanced skills needed to treat the most common causes of preventable death due to traumatic injuries include hemorrhage, from the extremities / junctional areas, tension pneumothorax, and airway trauma or obstruction. identify and treat other associated but not immediately life-threatening injuries.
- The Combat Medic/Corpsman (CMC) is the first medical provider to care for the casualty in the prehospital environment and is expected to provide more advanced care requiring significantly more medical knowledge and skills.
- The most advanced role is the Combat Paramedic/Provider (CPP) who are expected to provide the most sophisticated care to keep our wounded warriors alive and get them to definitive care.
Feedback from trainers and trainees indicated that the prior methods for TCCC training were heavy in PowerPoint slides and that more time performing procedures and applying those principles to realistic scenarios would be beneficial. Also, updates seemed to take months to make it to the field for implementation. Responding to that feedback, the decision was made to develop a web- and mobile-based platform for both classroom support and job performance support outside of the classroom. Deployed Medicine is the result of those efforts and is a continuously evolving platform where you can find classroom materials and other aids to learning more about TCCC.
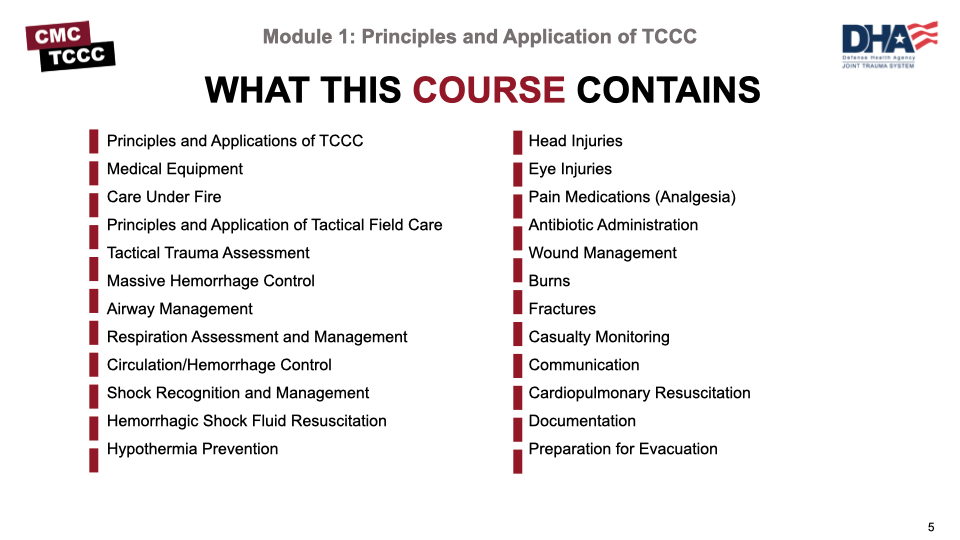
This CMC course is the evolution of what was previously known as the TCCC Medical Provider (TCCC-MP) course. This course includes additional objectives that the Joint Service Working Group, commissioned by the Defense Health Agency, the Committee on Tactical Combat Casualty Care, and Joint Trauma System, felt were important for CMC personnel. Below is a list of the different modules we will cover.
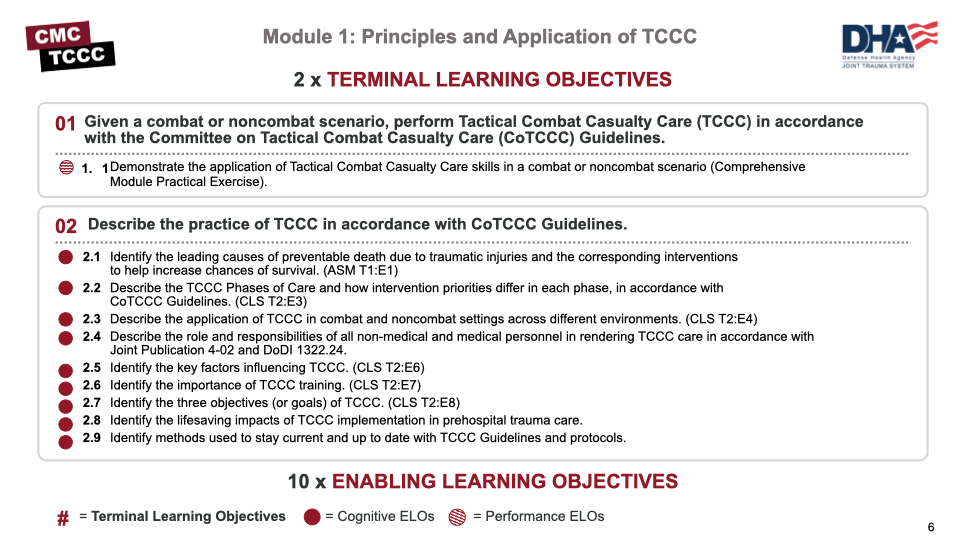
This first module will focus on the basic principles and application of TCCC. At the end of the course, you will be expected to demonstrate the application of TCCC skills in a practical exercise, and this module, along with those that follow, will set the stage for you to successfully complete that demonstration.
Throughout the course, you’ll see the enabling learning objectives listed as cognitive or psychomotor. The cognitive objectives are knowledge-based, while the psychomotor objects require that you learn and demonstrate a skill. The objectives for this first module are listed in the image below.
To help set the stage for this module, and for the course, let’s begin with an introduction video that overviews Tactical Combat Casualty Care (TCCC).
Intro to Tactical Combat Casualty Care (TCCC) Overview
The leading causes of preventable death due to traumatic injuries include hemorrhage, from the extremities / junctional areas, tension pneumothorax, and airway trauma or obstruction. By far, the majority of preventable deaths were from massive hemorrhage, and throughout this course, you will notice the emphasis on controlling bleeding, whether that be through tourniquet placement, the use of hemostatic dressings and wound packing, or the use of junctional tourniquets. But we still need to be cognizant of respiration and airway issues and be prepared to do Needle Decompressions of the Chest (NDC) or control the airway through airway maneuvers or advanced (minor surgical) airway maneuvers.
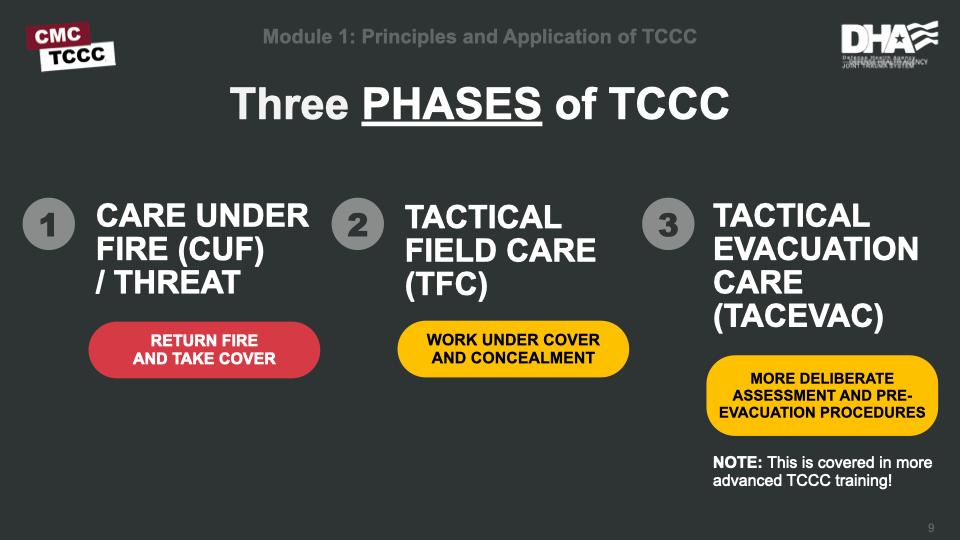
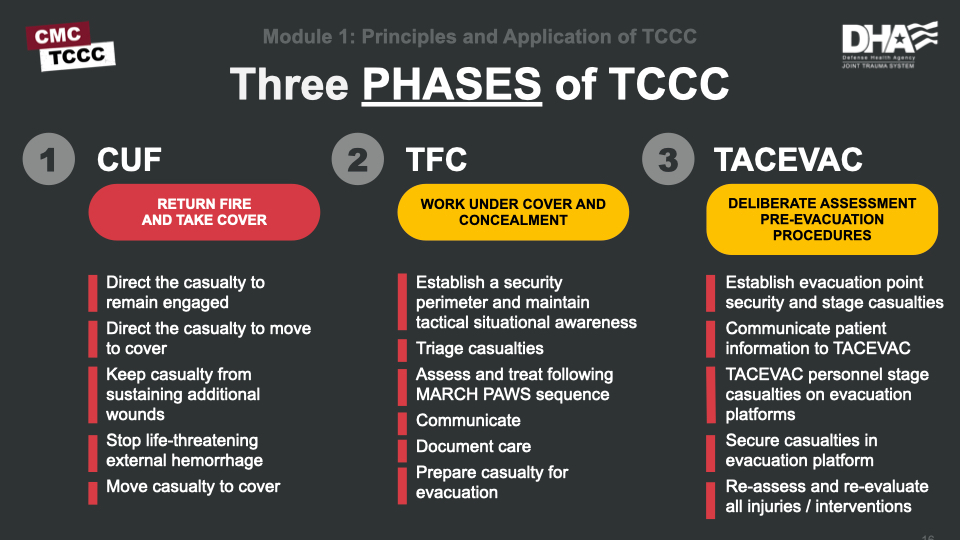
As you observed during the video, TCCC has three main phases of care: Care Under Fire (CUF)/Threat, Tactical Field Care (TFC), and Tactical Evacuation Care (TACEVAC). Each has specific considerations to keep in mind, both for the threats that may impact what care can be delivered and the priorities for treatment.
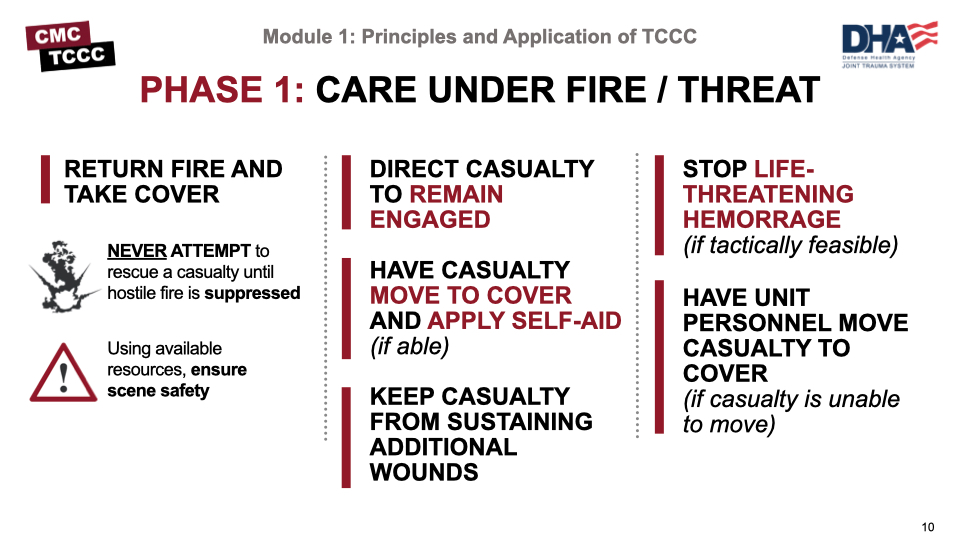
The first phase is Care Under Fire, or in the case of a noncombat environment, Care Under Threat. In this phase, the scene is not safe, and the overall priority is to establish scene safety in the form of fire superiority or control of any threats from a noncombat environment. The TCCC Guidelines state that the basic management plan for Care Under Fire is:
- Return fire and take cover.
- Direct the casualty to remain engaged as a combatant if appropriate.
- Direct the casualty to move to cover and apply self-aid if able.
- Try to keep the casualty from sustaining additional wounds.
- Stop life-threatening external hemorrhage if tactically feasible.
- Move the casualty to cover, if the casualty is unable to move.
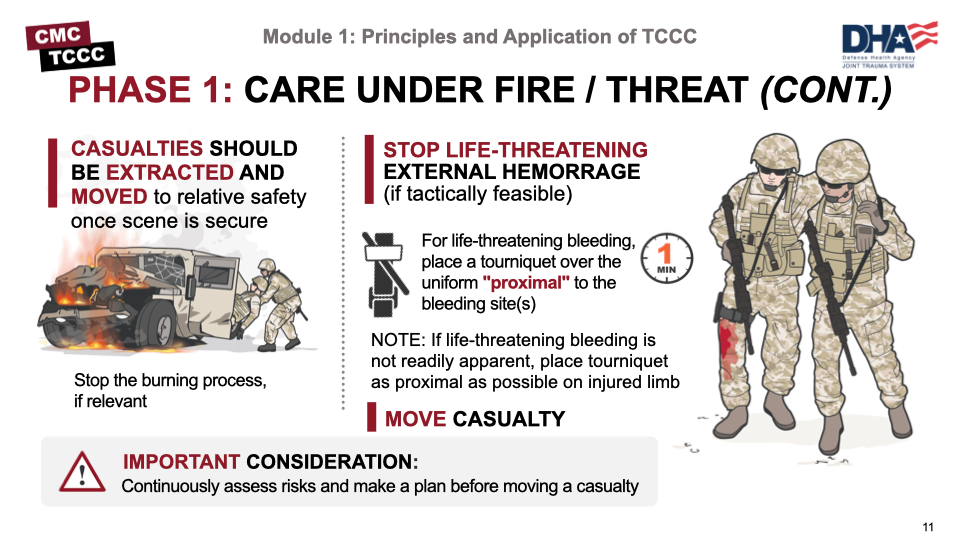
- Casualties should be extracted from burning vehicles or buildings and moved to places of relative safety. Do what is necessary to stop the burning process.
- Stop life-threatening external hemorrhage if tactically feasible:
- Direct casualty to control hemorrhage by self-aid if able.
- Use a CoTCCC-recommended limb tourniquet for hemorrhage that is anatomically amenable to tourniquet use.
- Apply the limb tourniquet over the uniform clearly proximal to the bleeding site(s). If the site of the life-threatening bleeding is not readily apparent, place the tourniquet “high and tight” (as proximal as possible) on the injured limb.
- Move the casualty to cover.
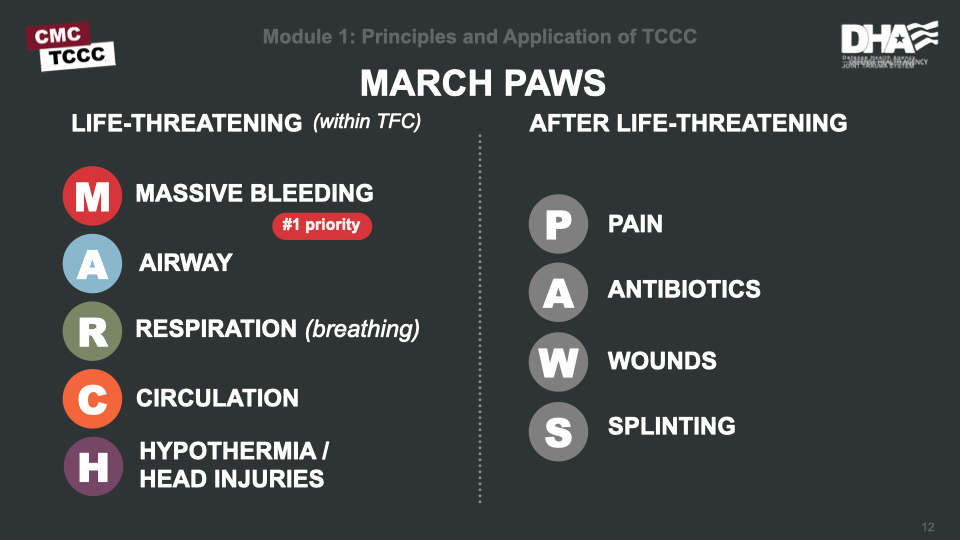
Before moving on to the Tactical Field Care phase, this is a good time to introduce the acronym MARCH PAWS approach and how it can help you decide on assessment and treatment priorities.
The MARCH sequence refers to issues with the potential for being life-threatening, all of which will be addressed in the Tactical Field Care phase. The order to approach them is also outlined by that sequence, beginning with massive bleeding. Any time your assessment reveals the need for an intervention or treatment, pause the assessment to complete the treatment and then resume the assessment where you left off.
The PAWS is also part of Tactical Field Care, if the tactical situation permits and/or if you have no other casualties that require your attention for immediate life-threatening issues. You’ll see this throughout the course, and it will also be helpful during your practical exercises.
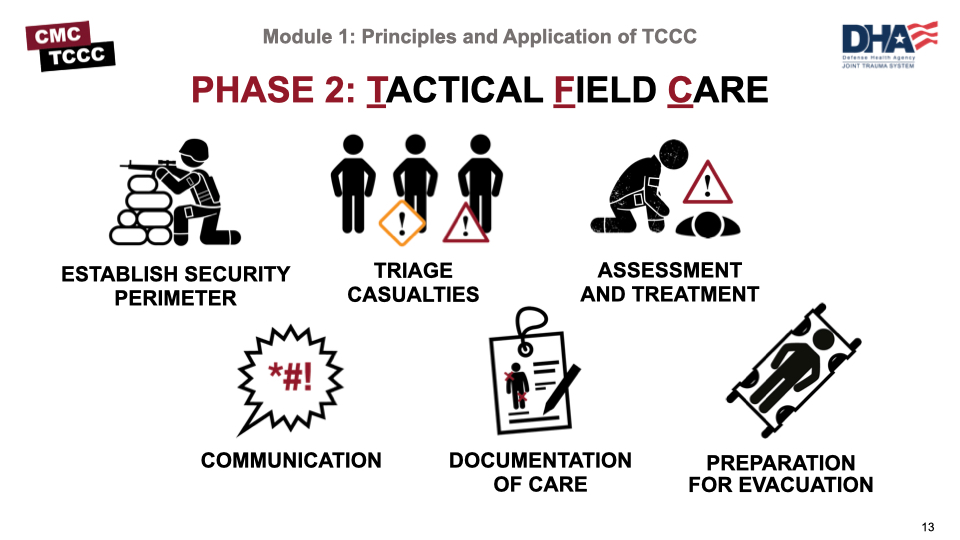
During Tactical Field Care, the TCCC Guideline basic management plan includes:
- Establish a security perimeter in accordance with unit tactical standard operating procedures and/or battle drills and maintain tactical situational awareness.
- Triage casualties as required. Casualties with an altered mental status should have weapons and communications equipment taken away immediately.
- Assessment and treat following the MARCH PAWS sequence.
- Communicate.
- Document care.
- Prepare for evacuation.
All of these will be covered in more detail in the modules that follow.
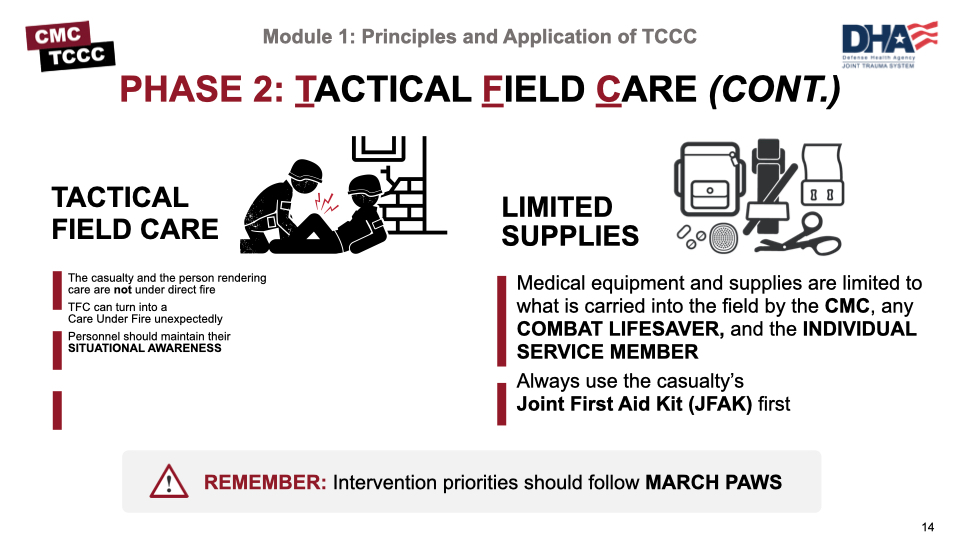
Keep in mind that Tactical Field Care can always revert to a Care Under Fire situation if scene safety is compromised. This is why there is such an emphasis on maintaining situational awareness of the surroundings and not using all of your resources to focus on casualty care.
Supplies in the field are usually limited. Exercise care by using the casualty’s JFAK initially; then use the supplies you have in your unit’s combat lifesaver kits (if available) and finally your CMC aid bag.
And, as always, be sure to prioritize your assessment and treatments by following the MARCH PAWS sequence we mentioned earlier.
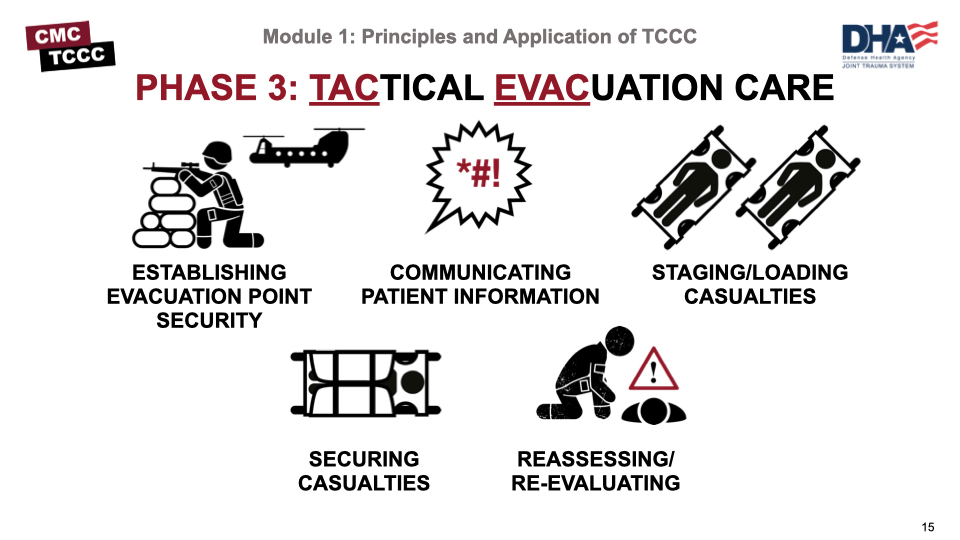
Basic Management Plan for Transition of Care to TACEVAC
Transition of Care from TFC
- Tactical force personnel should establish evacuation point security and stage casualties for evacuation.
- Tactical force personnel or the medic should communicate patient information and status to TACEVAC personnel as clearly as possible. The minimum information communicated should include stable or unstable, injuries identified, and treatments rendered.
- TACEVAC personnel should stage casualties on evacuation platforms as required.
- Secure casualties in the evacuation platform in accordance with unit policies, platform configurations and safety requirements.
- TACEVAC medical personnel should re-assess casualties and re-evaluate all injuries and previous interventions.
In summary, your casualty is likely to go through three distinct phases of care between point of injury and evacuation to a higher level of care. Each has different limitations and dictates different approaches to casualty assessments and treatments. Some of the key points are summarized in the following image. The individual modules you go through later in the course will have even more detail.
The principles of TCCC apply to trauma in both combat and noncombat settings. Severe bleeding or an amputation from a motor vehicle accident requires the same assessment and treatment you would render to a combatant who was injured from an IED blast. An active shooter produces the same ballistic injuries as an enemy combatant. Workplace accidents, vehicle rollovers, fires, explosions, burns, or other training accidents have accounted for a significant number of military noncombat injuries, all of which can be approached using the same principles of TCCC.
Although the principles of TCCC apply to trauma in both combat and noncombat settings, the environmental differences can play a significant role in how those principles are applied. For example:
- Hostile fire
- Darkness
- Environmental extremes
- Different wounding epidemiology
- Limited equipment
- Need for tactical maneuver
- Long delays to hospital care
- Different medic training and experience
If ballistic injury occurs in an urban setting with highly capable trauma surgery assets and rapid evacuation to a nearby civilian or military hospital, the issues surrounding assessment, treatment options, and casualty evacuation preparation will be very different than in an austere hostile setting, where a higher level of care is not readily available and responders are working in an austere location. TCCC Guidelines and training were developed assuming that most scenarios would lack nearby advanced trauma and evacuation assets.
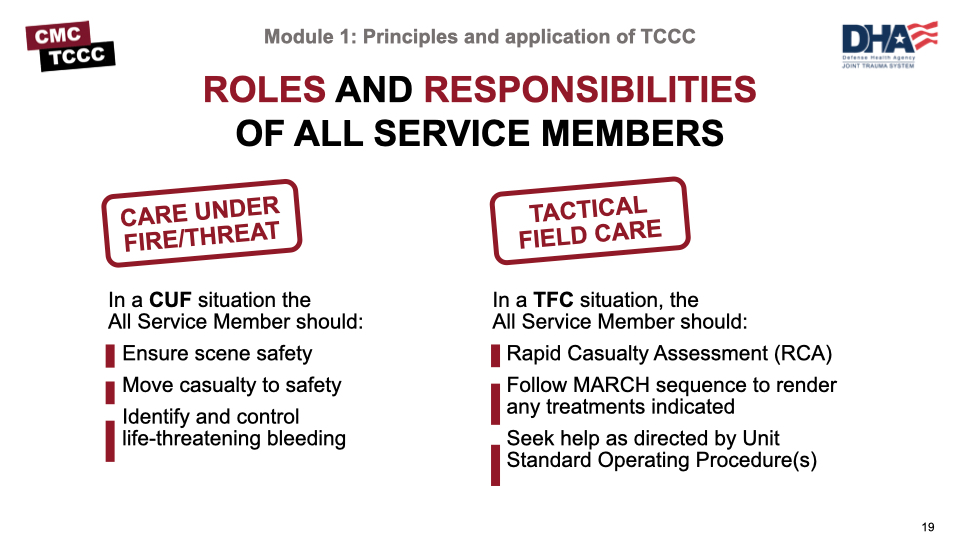
CMC personnel are not alone in providing medical care from the point of injury through evacuation to a more advanced role of care. All service members are required to have training in self-aid and buddy care. With the new Congressionally-mandated Medical Readiness Training instruction, this is changing from prior Service-specific (basic first aid) self-aid and buddy care training to the DHA standardized TCCC-All Service Member (ASM) course, although Services will still have additional medical training that they add based on their mission and risks associated in that environment.
In addition to the ASM personnel's basic understanding of the MARCH sequence, they will be trained on five lifesaving skills: RCA, tourniquet application, hemostatic dressing/wound packing, pressure bandages, and basic airway maneuvers.
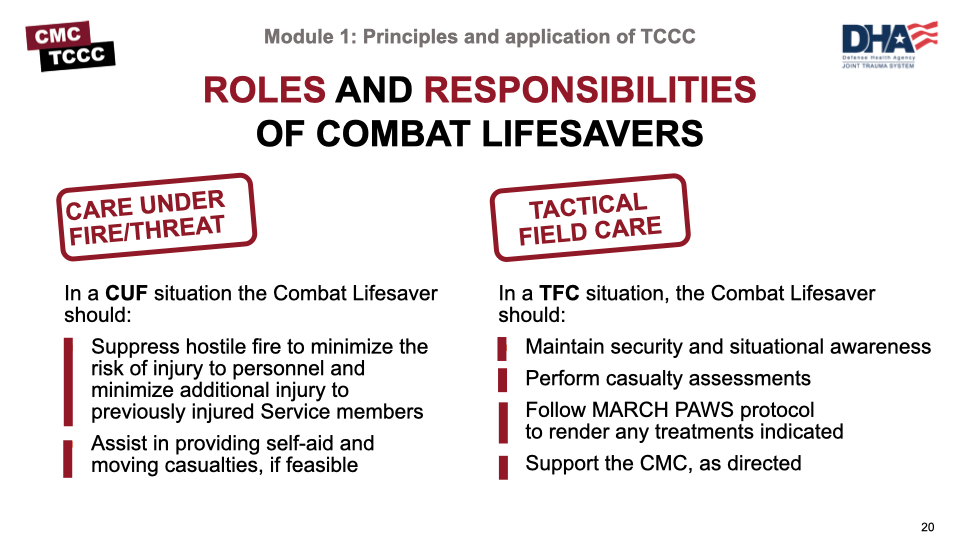
The combat lifesavers (CLS) are nonmedical military personnel with additional trauma training beyond basic first-aid procedures. The additional duties of combat lifesavers are to provide enhanced first aid for injuries based on their training before more advanced medical care arrives.
During the Care Under Fire phase, they will focus on gaining fire superiority and preventing further risk to casualties but can also apply self-aid principles and assist in casualty movement, if tactically feasible. In the Tactical Field Care phase, they can independently perform a casualty assessment and render any MARCH PAWS treatments that are indicated, although they may need to return to the fight if the situation changes. Also, the CLS can support CMC personnel and receive additional guidance and direction from them, as appropriate.
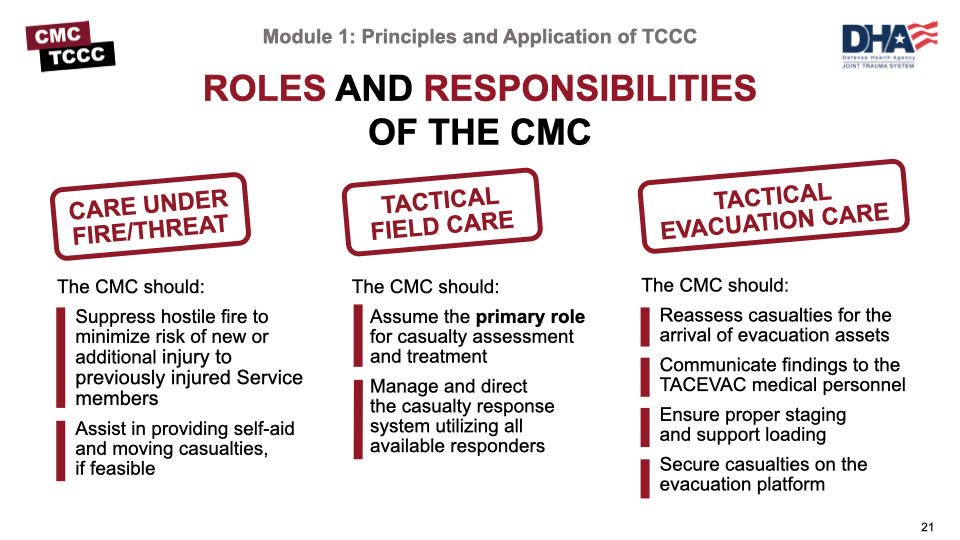
As a CMC, you are responsible for specialized first aid, triage, resuscitation, and stabilization, as well as casualty collection from the point of wounding and preparation of casualties for evacuation to a higher role of care.
In CUF, your role is to first suppress hostile fire like the CLS, but in TFC you assume the primary role for casualty assessment and treatment, following the TCCC Guidelines. In addition, manage and direct the casualty response system utilizing all available responders, providing guidance and direction to their activities. You are also responsible for preparing the casualties for evacuation.
In the TACEVAC phase, you are responsible for reassessing the casualties immediately before the arrival of the evacuation assets, communicating findings to the TACEVAC medical personnel, ensuring proper staging and supporting loading and securing of casualties on the evacuation platform.
All of these roles and responsibilities will be outlined in more detail over the remainder of the course.
Several factors influence the delivery of TCCC and are worth mentioning, as understanding them can help you prepare yourself and your CLS personnel to deliver better care.
In addition to environmental considerations (poor lighting, austere conditions, weather), you will usually be in a tactical environment that dictates your movements and communication options, as well as access to your support personnel and equipment.
If you are not under hostile fire, that risk is always present and requires some of your attention.
Depending on your mission profile, you may anticipate different wound patterns or threats.
In the best-case scenario, you will have had time to train and work with your ASM and CLS personnel, but that is not always the case.
Resupply can be erratic (or nonexistent) and tactical considerations may limit what you can take with you.
Finally, the potential for significant delays in evacuation may lead to prolonged field care issues.
It’s impossible to understate the value of training in TCCC. In addition to anecdotal stories about how TCCC has saved lives, irrefutable scientific evidence shows that TCCC principles will prevent deaths. Units that have mandated initial and sustained training requirements have been shown to have better retention of knowledge and skills, which will translate into improved performance in an operational setting.
Military units that have trained ALL of their members in TCCC have documented the lowest incidence of preventable deaths among their casualties in the history of modern warfare. In addition to the individual training on specific skills, unit-based training teaches the medical personnel and combat lifesavers/first responders how to work as a team, allowing them to be much more efficient when faced with a real-life situation.
Remember, the ongoing mission does not stop just because there is a casualty.
The three objectives of TCCC are to:
- Treat the Casualty - provide lifesaving care to the injured combatant
- Prevent Additional Casualties - limit the risk of taking further casualties
- Complete the Mission - enable the unit to achieve mission success
Tactical medical training historically was modeled on civilian courses like the Emergency Medical Technician (EMT) and Advanced Trauma Life Support (ATLS) courses and mirrored civilian trauma resuscitation guidelines, which provided excellent in-hospital care and results. But the principles they reflect often needed to be modified for the tactical setting, and that was not routinely done.
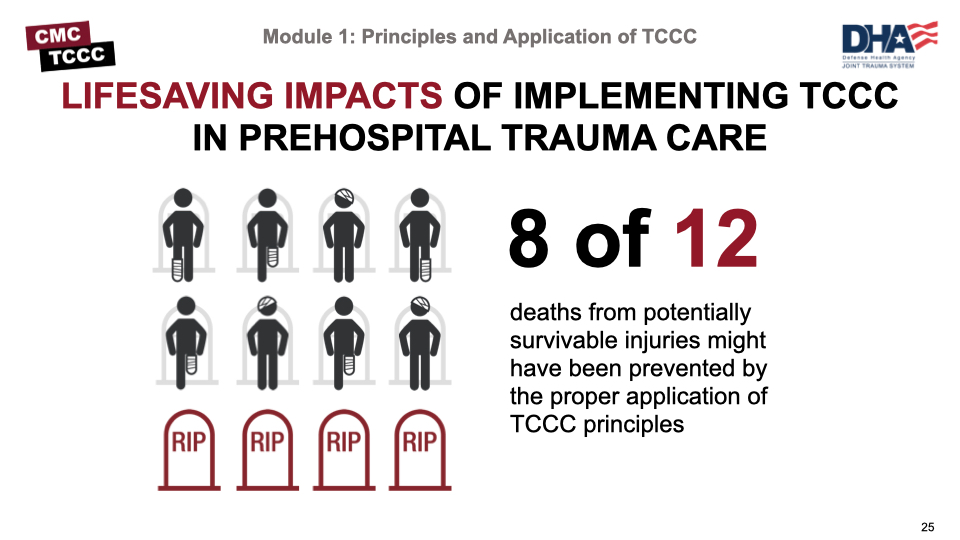
In previous conflicts, the use of tourniquets was discouraged, crystalloid fluid resuscitation was used for shock, hemostatic agents were not available, and airways were established through endotracheal intubation. At the start of the war in Afghanistan, TCCC was used only by a few innovative units in the US military. The impact of this limited use of TCCC was not well-appreciated until the first preventable death analysis was conducted. That study by Holcomb and others found that 8 of the 12 individuals who died from injuries that were potentially survivable might have been saved simply by the proper application of TCCC principles.
The experience with limb tourniquets was largely responsible for the adoption of TCCC throughout the US military. Tourniquets were a high-visibility issue for two reasons. First, tourniquet use was a radical departure from prehospital trauma care practice. Second, ubiquitous tourniquet use has clearly been the single most important lifesaving battlefield trauma care advance achieved during the wars in Iraq and Afghanistan.
The strategic messaging on tourniquets that drove the spread of TCCC from the Special Operations community to the conventional forces included reports of preventable death from extremity hemorrhage and documentation of improved survival as the use of extremity tourniquets became more prevalent. Now, in addition to evidence-based tourniquet guidance, many other TCCC advances have been adopted, such as hemostatic agents, Needle Decompression of the chest (NDC), advanced/surgical airways, resuscitation with blood products, and hypothermia prevention. These have not only had positive impacts on military prehospital trauma care but also have been widely adopted in the civilian community.
The need for periodic updates to the TCCC Guidelines was recognized early in the development of TCCC. The original TCCC paper recommended that the TCCC Guidelines be updated as needed by a Department of Defense-sponsored committee established for this purpose – the Committee on Tactical Combat Casualty Care, or CoTCCC.
Since the goal of TCCC is to provide the best possible medical care consistent with good small-unit tactics, it is essential that the membership of the CoTCCC include combat medical personnel as well as physicians. It is also critical to have Joint Service representation to ensure that differences in doctrine and experience between the Air Force, Army, Navy, and Marine Corps medical departments are identified and best practices from each are incorporated.
The tactical medical personnel selected for CoTCCC membership included Navy SEAL corpsmen, Navy corpsmen assigned to Marine units, Combat Medics, Ranger medics, Special Forces 18-D medics, Air Force pararescuemen (PJs), Air Force aviation medics, and Coast Guard health specialists. Physician membership included representatives from the trauma surgery, emergency medicine, critical care, and operational medicine communities. Physician assistants, medical planners, and medical educators are also represented.
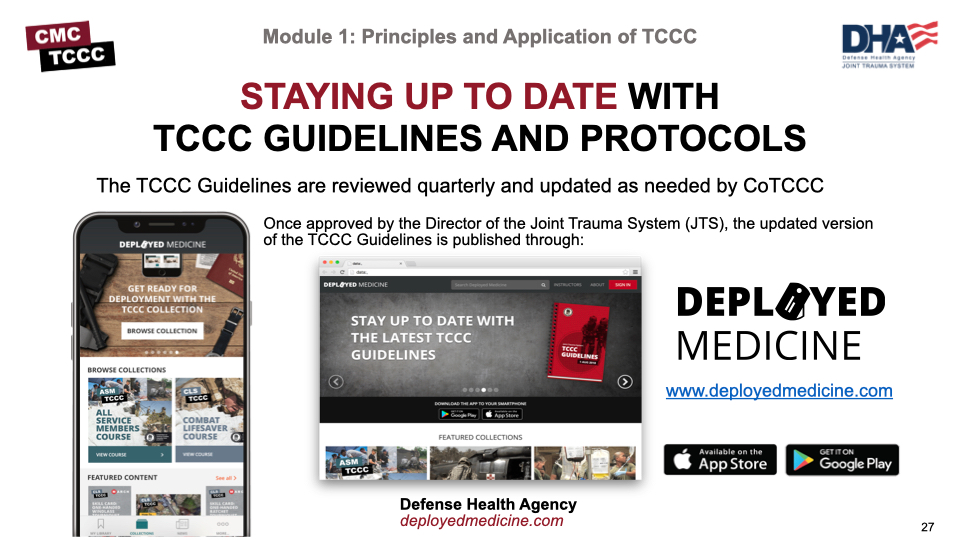
The TCCC Guidelines are reviewed quarterly and updated as needed by CoTCCC. The guidelines are published in a few places; however, Deployed Medicine is the official website to get the most up-to-date TCCC materials. Even though it is a .com website, it is an official site owned and managed by the Department of Defense. As soon as TCCC Guideline updates are approved for distribution by the Director of the Joint Trauma System (JTS), they will be updated directly onto Deployed Medicine.
Throughout the course, you’ll note several references, but keep in mind that the TCCC Guidelines are the core guidance for assessing and treating casualties in a TCCC setting, as well as the emphasis for training. Likewise, the Prehospital Trauma Life Support (PHTLS)., Military Edition, teaches and reinforces the principles of rapidly assessing a trauma patient using an orderly approach.
To close out this module, ask yourself about some of the factors that influence TCCC using the image below.
Answers
Which factors influence TCCC?
Hostile fire, tactical considerations, wounding patterns, environmental considerations, level of first-responder training and experience, equipment constraints and the potential for significant delays in evacuation.
What are the phases of care in TCCC?
Care Under Fire/Threat, Tactical Field Care, and Tactical Evacuation Care.
What is the most essential treatment task in CUF?
Application of a limb tourniquet to control massive bleeding.
What is every first responder’s role in CUF?
Suppress hostile fire and/or establish scene safety, assist in self-aid, and assist in moving casualties, if feasible.
What does MARCH PAWS stand for?
Massive bleeding, airway, respirations (breathing), circulation, and hypothermia AND head injury, pain, antibiotics, wounds, and splints.