TFC Airway
JTS / CoTCCC
Introduction
Tactical Field Care is the care rendered by the first responder or combatant once no longer under effective hostile fire. It also applies to situations in which an injury has occurred, but there has been no hostile fire. Available medical equipment is still limited to that carried into the field by unit personnel. Time to evacuation to a medical treatment facility may vary considerably. Tactical field care allows more time and a little more safety, to provide further medical care.
But Remember – effective hostile fire could resume at any time.
After completing the Hemorrhage Control portion of Tactical Field Care, you will shift your focus to the casualty's airway and respirations. When managing the airway during TFC you should disarm any casualty with an altered state of consciousness and secure communications and sensitive mission items. This module will show you how to open the airway with either a chin lift/jaw thrust, nasopharyngeal airway, or by placing the casualty in the recovery position. If these methods are ineffective, consider performing a surgical airway.
Objectives
Videos
Guidelines and Key Points
Triage casualties as required.
Casualties with an altered mental status should immediately have weapons cleared and secured, communications secured, and sensitive mission items redistributed.
Possible causes of altered mental status are Traumatic Brain Injury (TBI), shock, hypoxia, and pain medications. The casualty may resist being disarmed. It may be useful to say “Let Smith hold your weapon for you while I check you out,” to help them better accept your taking their weapon.
Airway Management
1. Conscious casualty with no airway problem identified:
- No airway intervention required
2. Unconscious casualty without airway obstruction:
- Chin lift or jaw thrust maneuver or
- Nasopharyngeal airway or
- Extraglottic airway
- Place casualty in the recovery position
3. Casualty with airway obstruction or impending airway obstruction:
- Allow a conscious casualty to assume any position that best protects the airway, to include sitting up
- Use a chin lift or jaw thrust maneuver
- Use suction if available and appropriate
- Nasopharyngeal airway or
- Extraglottic airway (if the casualty is unconscious)
- Place an unconscious casualty in the recovery position.
4. If the previous measures are unsuccessful, perform a surgical cricothyroidotomy using one of the following:
- Cric-Key technique (Preferred option)
- Bougie-aided open surgical technique, using a flanged and cuffed airway cannula of less than 10 mm outer diameter, 6-7 mm internal diameter, and 5-8 cm of intratracheal length
- Standard open surgical technique using a flanged and cuffed airway cannula of less than 10 mm outer diameter, 6-7 mm internal diameter, and 5-8 cm of intra-tracheal length (Least desirable option)
- Use lidocaine if the casualty is conscious.
5. Cervical spine stabilization is not necessary for casualties who have sustained only penetrating trauma.
6. Monitor the hemoglobin oxygen saturation in casualties to help assess airway patency.
7. Always remember that the casualty’s airway status may change over time and requires frequent reassessment.
- The recovery position helps to protect against vomiting and aspiration. Again, note that C-spine stabilization is not required in penetrating head and neck trauma.
- Casualties with severe facial injuries can often protect their own airway by sitting up and leaning forward. Let them do it if they can. You may have to do a surgical airway with the casualty in the sitting position.
- The i-gel is the preferred extraglottic airway because its gel-filled cuff makes it simpler to use and avoids the need for cuff inflation and monitoring. If an extraglottic airway with an air-filled cuff is used, the cuff pressure must be monitored to avoid overpressurization, especially during TACEVAC on an aircraft with the accompanying pressure changes.
- Extraglottic airways will not be tolerated by a casualty who is not deeply unconscious. If an unconscious casualty without direct airway trauma needs an airway intervention, but does not tolerate an extraglottic airway, consider the use of a nasopharyngeal airway.
- For casualties with trauma to the face and mouth, or facial burns with suspected inhalation injury, nasopharyngeal airways and extraglottic airways may not suffice and a surgical cricothyroidotomy may be required.
- Surgical cricothyroidotomies should not be performed on unconscious casualties who have no direct airway trauma unless use of a nasopharyngeal airway and/or an extraglottic airway have been unsuccessful in opening the airway.
Cricothyroidotomy is hard to do. Combat medics have often failed to get it right on the battlefield, with a 33% failure rate. This is the most technically difficult procedure we ask medics, corpsmen, and PJs to do.
The Cric-Key is the preferred surgical airway technique. Under test conditions, medics were faster and more successful using the Cric-Key technique compared to the open surgical technique.
To prepare, combat medics should perform a cricothyroidotomy at least five times during training on an anatomically realistic model.
Summary
Analysis of Battlefield Cricothyroidotomy in Iraq and Afghanistan
Robert L. Mary, MD; Alan Frankfurt, MD
The Journal of Special Operations Medicine
J Spec Oper Med. 2012 Spring;12(1):17-23.
Historical review of modern military conflicts suggests that airway compromise accounts or 1-2 % of total combat fatalities. This study examines the specific intervention of pre-hospital cricothyrotomy (PC) in the military setting using the largest studies of civilian medics performing PC as historical controls.
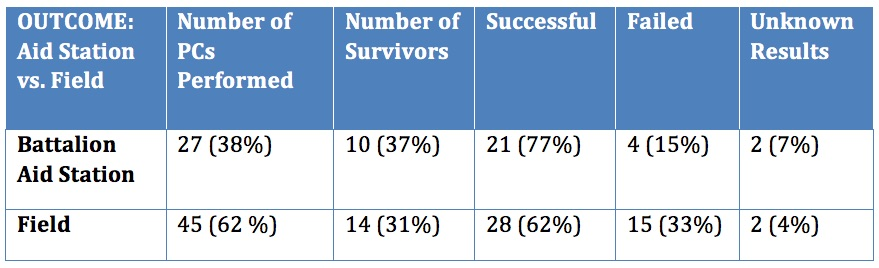
The majority of patients who underwent PC died (66%). The largest group of survivors had gunshot wounds to the face and/or neck (38%) followed by explosion related injury to the face, neck and head (33%). Military medics have a 33% failure rate when performing this procedure compared to 15% for physicians and physician assistants. Minor complications occurred in 21% of cases. The survival rate and complication rates are similar to previous civilian studies of medics performing PC. However, the failure rate for military medics is three to five times higher than comparable civilian studies.
Take Home Message:
Comparison of Two Open Surgical Cricothyroidotomy Techniques by Medics using a Cadaver Model
Robert L. Mary, MD; Alan Frankfurt, MD
The Journal of Special Operations Medicine
J Spec Oper Med. 2012 Spring;12(1):17-23.
The CricKey is a novel surgical cricothyroidotomy device combining the functions of a tracheal hook, stylet, dilator, and bougie incorporated with a Melker airway cannula. This study compares surgical cricothyroidotomy with standard open surgical versus CricKey technique.
Participants included US Army combat medics credentialed at the emergency medical technician–basic level. After a brief anatomy review and demonstration, 15 military medics with minimal training performed in random order standard open surgical cricothyroidotomy and CricKey surgical cricothyroidotomy on cadavers. Compared with the standard open surgical cricothyroidotomy technique, military medics demonstrated faster insertion with the CricKey. First-pass success was not significantly different between the techniques.


READ FULL PDF
Take Home Message:
Chest Wall Thickness in Mil Personnel: Implications for Needle Thoracentesis in Tension Pnemothorax
COL H. Theodore Harcke, MC USA, COL H. Theodore Harcke, MC USA; LCDR Lisa A. Pearse, MC USN; COL Angela D. Levy, MC USA; John M. Getz, BS; CAPT Stephen R. Robinson, MC USN
Military Medicine, Vol. 172, December 2007
Advanced Trauma Life Support guidelines and combat casualty care doctrine recommend the use of needle thoracentesis (needle thoracostomy) for the emergency treatment of tension pneumothorax. Emergency situations require a reproducible, simple, and effective normal response for treatment of life-threatening pneumothorax. This study evaluated chest wall thickness in a forward-deployed tri-service population using a retrospective analysis of multidetector CT (MDCT)-assisted autopsies performed on combat casualties at the Armed Forces Institute of Pathology.
If needle thoracentesis is attempted with an angiocatheter or needle of insufficient length, the procedure will fail. Recommended procedures for needle thoracentesis to relieve tension pneumothorax should be adapted to reflect use of an angiocatheter or needle of sufficient length. A 3.25 inch angiocatheter would have reached the pleural space in 99% of the cases in this series.

READ FULL PDF
