U. S. Central Command COVID-19 Pandemic Playbook for Operational Environments
U.S. Central Command
U.S. Central Command COVID-19 Pandemic Playbook for Operational Environments Version 3
Contributors
Leads: Maj Mary Stuever, MAJ Ashley Hydrick, Dr. Patricia Meza, COL Tamara Funari
CDR Stephanie Bedzis
Col. J. Scott Calder
CDR R. Christopher Call
Maj Rebecca Castañeda
COL Amal Chatila
Lt Col Vicki Charbonneau
LTC Sally Delvecchio
CDR Bambi Pish-Derr
Ms. Patricia Drouillard
CDR Nichole Dutton
LTC Jennifer Edmundson
Dr. Erin Eickhoff
LTC Jennifer Gomes
Lt Col Andrew Hall
LTC Fred Hauser
Mr. C. Ray Huntsinger
Dr. Sean Keenan
COL Donald Kimbler
Ms. Linda Martinez
Ms. Lisa McFarlan
CPT Rachel Patrick
MSG Michael Remley
LTC Johnnie Robbins
Ms. Laura Runyan
Dr. Elizabeth Mann-Salinas
Mr. Phil Sartin
Col Stacy Shackelford
LTC Tom Sherbert
Mr. Jim Sjovall
Dr. Kimberly Smith
Lt Col Steffanie Solberg
This playbook is aimed at healthcare, public health providers, and staff in the United States Central Command (USCENTCOM) Area of Responsibility (AOR). The USCENTCOM AOR is a medically austere operational environment where Role 3 (R3) is the highest level of medical capability. All planning assumptions proceed from there. This playbook is a concise source of key information, references, and materials for providers and healthcare leaders to easily review. The playbook is comprehensive but not all inclusive, and does not negate the need for communication and information sharing with local, Joint Task Force (JTF), Service Component and USCENTCOM Headquarters (HQ) Command and Surgeon Cells.
Additions & Revisions
Revisions and updates were completed throughout this document to be current as of 23 Apr 2021. Major additions and revisions include:
- Updated information on guidelines for Force Health Protection, to include: isolation and quarantine, including discharge and return to duty guidelines
- Added information on testing for general screening and diagnostic testing
- Added information on the new COVID vaccination
- Added information on the treatments for COVID
- Added updates for patient tracking in theatre
- All other revisions involve addition of resource links throughout and minor refinement of language for clarity and grammar
This document provides key information in text and graphic images for rapid review. The Table of Contents will link users to the topic they want to review, which will contain key facts and figures, as well as linking users to external resources that can provide greater detail. Users are encouraged to use this playbook as a tool to connect to best practice resources that will augment existing clinical and military expertise and local, JTF, Service Component, and USCENTCOM guidance.
- AE Patient Classification: A basic metric to convey patient acuity and level of infectivity to others. Patient classification will be performed in accordance with the Department of the Air Force Instruction DAFI 48-107, EN Route Care Documentation, Volume 3, 17 Dec 2020.
- Airborne Spread: Spread of disease via small liquid particles (aerosols) that remain aloft for prolonged periods of time and may travel longer distances. Airborne precautions aim to mitigate this method of transmission.
- Antibody: Proteins produced by infected individual as part of their immune response to infection by the pathogen.
- Antigen: Proteins or other cellular or chemical features associated with the pathogen (e.g., viral DNA, surface proteins).
- Close Contact: Close contact is defined by the Centers for Disease Control and Prevention (CDC) as someone who was within 6 feet of an infected person for a cumulative total of 15 minutes or more over a 24-hour period starting from 2 days before illness onset (or, for asymptomatic patients, 2 days prior to test specimen collection) until the time the patient is isolated.
- Contact Spread: Spread of disease via direct contact with an infected patient or contaminated surface. Contact Precautions aim to mitigate this method of transmission.
- Droplet Spread: Spread of disease via relatively large liquid particles that settle from the air quickly (within a few feet). Droplet Precautions aim to mitigate this method of transmission.
- Intermediate Care Ward (ICW): An inpatient nursing unit that typically accommodates patients requiring med surgical to progressive (step-down) – level care. In pandemic conditions, this definition may broaden to incorporate levels of care similar to mass casualty. Staffing considerations and Knowledge, Skills and Abilities (KSAs) will be commensurate with the roles required. The mission may require staff to increase their KSAs. Additional considerations may be needed for patients requiring isolation. In a crisis environment, all staff are asked to work at the top of their license.
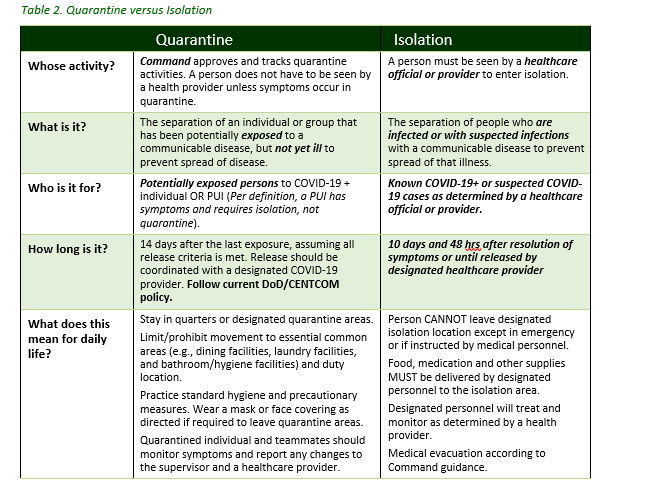
- Isolation: The separation of an individual or group infected or reasonably believed to be infected with a communicable disease from those who are healthy in such a place and manner to prevent the spread of the communicable disease. Isolation is a medical term and ordered by a medical provider, but requires command support for successful execution.
- Pathogen: an organism that causes disease (e.g. virus, bacteria, fungus, or parasite). The term is also used to describe prions – non-living protein particles that display infectious behavior.
- Patient Under Investigation (PUI): A patient with signs and symptoms consistent with known possible presentations of COVID-19 with potential exposure to the virus. Potential exposure to the virus is defined as close contact with known or other suspected cases and/or travel through regions with widespread sustained transmission of COVID-19. In areas where COVID-19 is already widespread, symptoms alone may make the diagnosis of “PUI.” A PUI may refer to: 1) an individual whose diagnostic testing has not yet been performed, 2) an individual with symptoms consistent with COVID-19 but diagnostic testing is unavailable, or 3) an individual with high index of suspicion for COVID-19 whose initial COVID test was negative. All PUIs must be isolated. All patients being admitted to the hospital for suspected COVID are considered PUIs until tested for COVID.
- Quarantine: The separation of an individual or group that has been potentially exposed to a communicable disease, but is not yet ill, from others who have not been so exposed, in such a manner and place to prevent the possible spread of the communicable disease. This is a form of Restriction of Movement (ROM) and is a command function that is medically supported. Quarantine is a commander’s responsibility.
- Social Distancing: The practice of reducing close contact between people to slow the spread of disease. It includes: wearing masks that cover the nose and mouth, limiting large group gatherings (no more than 10 persons), closing buildings and gathering spaces, cancelling events, and advising people to stay six feet apart as much as possible. Preparation of isolation berthing, including activities of daily living (e.g., hydration, food, hygiene, trash disposal) is addressed on pages 25-26 of the COVID-19 CPG for Austere Operational Environments.
AE - Aeromedical Evacuation
AFMES - Air Force Medical Examiner System
AOR - Area of responsibility
C2 - Command and Control
CENTREX COVID tracker: using this system to track patients.
CJTF - Combined Joint Task Force
CCIR - Commander’s Critical Information Reporting
CCOP - Central Command Operating Procedures
CCSG - Command Surgeon
CHU - Containerized Housing Unit
CONOPS - Concept of Operations
CONPLAN - Concept of Operations Pan
CSOC - Crisis Standards of Care
DHA - Defense Health Agency
EXORD - Executive Order
FFR - Filtering Facepiece Respirators
HIPAA - Health Insurance Portability and Accountability Act
HPCON - Health Protection Conditions
ICW - Intermediate Care Ward
KSA - Knowledge, Skills and Abilities
MS - Medication Safety
MSAT - Medical Situational Awareness in the Theater
MWR - Morale Welfare and Recreation
PHEO - Public Health Emergency Officer
PHEM - Public Health Emergency Management
PFA - Psychological First Aid
PMG - Practice Management Guide
PPE - Personal Protective Equipment
PS - Patient Safety
PUI - Person Under Investigation
QS - Quality and Safety
SIPRNet - Secret Internet Protocol Router Network
SME - Subject matter expert
TPMRC-E - Theater Patient Movement Requirements Center East
USCENTCOM – United States Central Command
USTRANSCOM - U.S. Transportation Command
VITAL-T - Virtual Inspection and LINKUP in Theater
VH - Virtual Health
The USCENTCOM CONPLAN 1251-15, Regional Concept Plan for Preparation and Response for Pandemic Influenza and Infectious Disease (PI&ID), delineates the policies, actions and requirements for the employment of military resources within the USCENTCOM AOR for PI&ID preparation and response plan, along with other plans, are available for download on the USCENTCOM SIPRnet website. You can also reach the SIPRNet through https://ccsg.nonrel.centcom.smil.mil/Private/SitePages/Home.aspx and click on the COVID-19 link. There will be links to EXORDS and instructions. Refer to CCJ3 for assistance if copies of instructions are needed.
Specific Health Service Guidance is delineated in the Annex Q to the USCENTCOM EXORD Novel Coronavirus Outbreak Response Operations in the UCENTCOM SIPRNet link.
An excellent summary of medical operational experiences was authored by Task Force Medical (TFM) 14. The Memorandum for record: Role 3 Standard Operating Procedure (SOP) for Coronavirus (COVID-19) Triage and Admission Criteria, 18 Aug 2020, provides guidelines for TFM 14 Role 3 responsibilities while caring for suspected COVID-19 positive patients.
Coordination is essential between Command Staff, medical teams, and public health/preventive medicine assets. Given the highly complex nature of the COVID-19 disease and need for subject matter expertise (SME), Commanders are encouraged to designate a COVID-19 response and planning team consisting of medical and public health/preventive medicine SMEs along with operational planners. Task Force Med Leaders are encouraged to coordinate with respective Surgeon teams and Force Health Protection assets to translate and communicate all guidance and policy down to the most forward units with attention to operational security and patient privacy laws. In order to facilitate a coherent Joint effort, the response should follow established DoD procedures as outlined in DODI 6200.03 Public Health Emergency Management (PHEM) Within the DoD, 28 Mar 2019 and DODI 6055.17 DoD Emergency Management (EM) Program, Change 3 effective 12 Jun 2019.
All leaders should operate under a number of considerations/assumptions including (but not limited to):
- Command and Control (C2) authorities will remain unchanged unless otherwise directed. Combined Joint Task Force Surgeon (CJTF) and Component Surgeon cells should continue to collaborate and communicate closely with higher headquarter authority and disseminate information to the most forward units.
- Current USCENTCOM missions will continue, unless otherwise directed, throughout the COVID-19 pandemic, daily tasks may need to be reprioritized as required by a pandemic response to maintain surgical and critical care capabilities while minimizing spread of infectious disease in theater.
- Leaders are encouraged to collaborate and delegate authority to improve comprehensiveness planning and operation activities. Subordinate leaders should be empowered to utilize their expertise and innovation within the boundaries set-forth by pre-established policy and guidance. The USCENTCOM Health Protection Condition (HPCON) Checklist, Joint Force Health Protection Team, COVID-19 Crisis Action Team (when available) will assist appropriate actions listed in Appendix A.
- Communication is key for interdisciplinary COVID-19 planning and response. Limit jargon and clearly define all acronyms and unfamiliar terms, for example. Commanders should communicate key information to subordinate units.
- Logistical and patient movement channels are likely to be altered by the pandemic both in theater and at receiving Role 4 Contiguous United States (CONUS) and Outside the Contiguous United States (OCONUS) facilities. These challenges must be overcome by clear communication and adaptive planning strategies.
RESOURCES
Refer to Headquarters, CJTF, and Component guidance for specific information and requirements with regards to operational planning guidance.
The U.S. Department of Health and Human Services provides Critical Care Planning-COVID-19 Quick Notes a two-page document which describes operationalization of the concept in three major categories: space, staff, supplies, and provision of critical care.
Planning and Preparation, pg6, Implications of COVID-19 on Surgical Care, p8, DoD COVID-19 PMG v7.0, 03 Mar 2021.
COVID-19 Response and Prevention Planning-Knovel (Elsevier)
DODI 6200.03 Public Health Emergency Management (PHEM) Within the DoD, 28 Mar 2019
DODI 6055.17 DoD Emergency Management (EM) Program, Change 3 effective 12 Jun 2019
All USCENTCOM bases and facilities should establish a local and regional PACE (Primary-Alternate-Contingency- Emergency) plan for both operational and clinical communication incorporating social distancing and division of labor during the pandemic response period.
The USCENTCOM Component and CJTF teams may have prospectively published local and regional PACE plans for both operational and clinical consultation and communication. Forward-stationed medical teams/medics should identify and test these options PRIOR to needing urgent consultation.
Division of labor and social distancing could strain all routine secure and unsecure DoD communication and collaboration platforms (i.e. teleconferencing video conferencing networks, remote access email), resulting in the incorporation of non-DoD unsecure platforms (e.g., Zoom, Skype, WhatsApp). Operational security and patient privacy must be a primary consideration when selecting communication platforms, especially when using non-DoD platforms.
UPDATE 2.0: In answer to the social distancing challenge in the work place, the DoD has established an approved virtual communication platform to improve personnel connection and information sharing. This platform is approved for controlled unclassified information sharing and is noted HIPAA compliant. It connects with individuals’ regular Non-classified Internet Protocol Router (NIPR) email accounts for ease of communications and scheduling. For more information on how to get connected visit the following link through June 2021: https://www.cloud.mil/CVR/.
RESOURCE
Refer to the Planning and Preparation, p12, DoD COVID-19 PMG v7.0, 3 March 2021
Documentation of patient care and movement should continue via the usual platforms (i.e. paper or electronic charts) as previously established at the local treatment facility. The appropriate ICD-10 codes, and symptoms (e.g. fever, cough and shortness of breath), should be entered as detailed as possible in order to capture these patients in Theater Medical Data Store (TMDS), Medical Situational Awareness in the Theater (MSAT) and Medical Combined Operating Picture (MEDCOP) and future databases and overall future performance improvement opportunities.
JTS has published the ICD-9 and ICD-10 Codes to accompany the new COVID-19 registry under development. The codes can be found on the following JTS website: https://jts.amedd.army.mil/assets/docs/education/COVID-19_ICD-9_ICD-10_Codes.pdf Please ensure that outpatient encounters are closed at the end of the patient encounter (i.e. when the patient departs medical facility).
All patients, staff, and support personnel with symptoms (fever, cough, shortness of breath) should be tested for COVID-19 using the available confirmatory diagnostic test.
All persons who test positive need to be moved into isolation and if medical management is required, considered for evacuation to OCONUS or CONUS locations as designated for the evacuation plan per that region (follow the guidance provided in the Transport section of this Playbook).
Command and medical teams are responsible for establishing a plan for patient tracking and re-unification (for family notification of patient status) locally. In accordance with USCENTCOM regulations, local Commanders will include COVID-19 patient tracking as part of their Commander's Critical Information Reporting (CCIR). Patient tracking for the USCENTCOM AOR will be accomplished using SIPR COVID-19 CAT SharePoint/Trackers & Updates/Patient Trackers by Component.
The JTS has partnered with the Uniformed Services University of Health Sciences (USU) to develop a registry for COVID-19 patient data acquisition. Detailed documentation including appropriate ICD-10 codes are essential to assist key term triggers for audits. If using hard copy/paper charting, all documentation should be uploaded to Theater Medical Data Store as soon as possible.
The JTS COVID registry will ease tracking and monitoring the progress of this disease process, while evaluating the quality and possibility for improvement of delivery of care. In the meantime, units should designate a person responsible for tracking and monitoring the COVID-19 patient care and patient movement. The JTS COVID-19 Registry is the only approved data repository for CENTCOM.
For information email: DHA.JBSA.j-3.List.JTS-PIP@mail.mil (JTS PI team).
The following list provides the intermediate and after action reviews that provide important sources for sharing best practices and innovative ideas to enhance performance improvement:
- COVID-19 Monitoring and Response Among U.S. Air Force Basic Military Trainees — Texas, March–April 2020, MMWR, 05 June 2020.
- COVID-19 in Erbil Air Base: Lessons Learned Managing Multiple COVID-19 Outbreaks at a Deployed, Austere Location (See Appendix E: COVID-19 in Erbil Air Base Executive Summary).
Transport guidance has changed frequently and is ever changing with the current environment. Check with local Operations cell to ensure most current guidance is followed. As of the date of this publication:
- All patients with symptoms severe enough to require admission to a medical facility for symptom management and/or supplemental oxygen should be considered for evacuation.
- Host Nation admitted patients may remain in hospital at commander’s discretion.
- Navy Afloat remains on ship unless ship’s capability is in danger of being exceeded (either by volume or the severity of the patient.)
- Asymptomatic COVID+ or mildly symptomatic patients should stay but a commander may decide to evacuate.
For patients with a new (+) COVID test within 72 hours of patient transport by AF Aeromedical Evacuation (AE/CCATT) or civilian air ambulance, in addition to usual contact tracing procedures, please notify the regional TRANSCOM Patient Movement Requirements Center (TPMRC) that services that MTF (TPMRC-A DSN (312) 779-4200, TPMRC-E DSN (314) 480-8040, TPMRC-W DSN (315) 448-1609); the U.S. Transportation Command (USTRANSCOM) Instruction 41-02, 11 July 2019 outlines Patient Movement of Contagious and potentially exposed casualties. This playbook is a summary that pertains specifically to COVID-19. The guidance for movement and evacuation of COVID-19 positive patients is rapidly evolving. Early and close coordination of these movement requests with Theater Patient Movement Requirements Center East (TPMRC-E) and next higher headquarters is crucial.
To ensure correct resource allocation and transport prioritization, units should refrain from using locally derived patient categorization. Patient classification should remain IAW DAFI 48-107, EN ROUTE CARE DOCUMENTATION, Volume 3, 17 December 2020.
Movement of multiple COVID-19 patients will be performed using a DoD certified and approved contagious patient movement system. Planning considerations must take into account downtime for decontamination of aircraft following COVID-19 patient evacuation. Upon consultation and appropriate approvals, capabilities developed outside of the DoD for moving patients exposed to or infected with COVID-19 may be used for approved missions via commercial aircraft. The sending MTF must coordinate movement with TPMRC-E for both intra and inter-theater PM.
Refer to local, CJTF, Component, and USCENTCOM guidance for specific knowledge on Operational Planning assumptions, considerations and guidance located on the USCENTCOM Surgeon (CCSG) SharePoint.
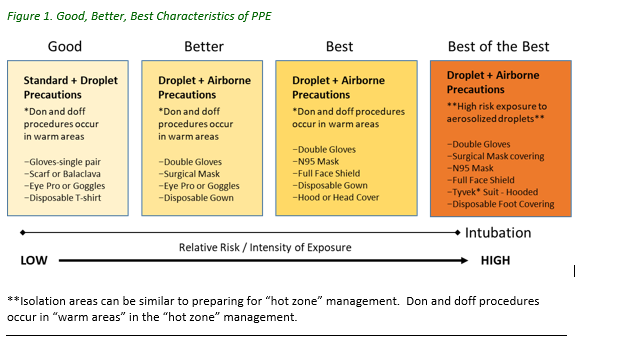
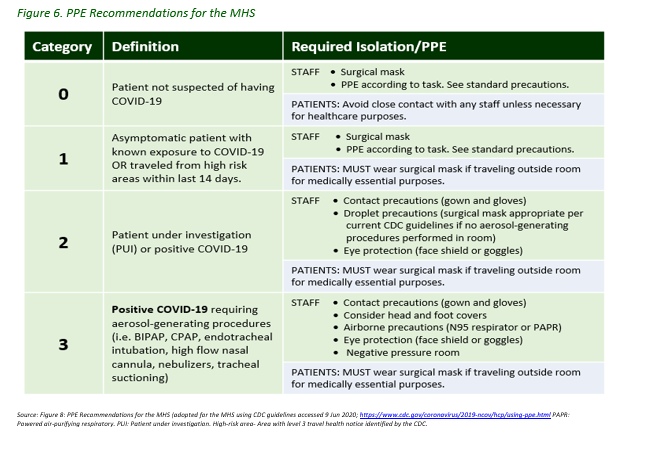
COVID-19 is a respiratory virus that requires up to advanced droplet (droplet/airborne) precautions depending on the risk of activity (below). All re-use and extension of PPE MUST be done in accordance with CDC, JTS, and USCENTCOM best practices and guidance.
RESOURCES:
USCENTCOM Infection Prevention and Control Policy in a Deployed Setting or service component site such https://portal.arcent.swa.army.mil/covid19opt/SitePages/Home.aspx
USCENTCOM policies align with CDC guidance. Capabilities are limited in the AOR by the types of equipment available. The following CDC links provide updated guidance:
Employed cleaning protocols should ensure adequate sanitization in all environments, including quarantine/isolation/patient care areas, as well as all workspaces and quarters. All non-dedicated, non-disposable patient care medical equipment should be cleaned and disinfected according to manufacturer’s instructions and facility policies. The U.S. Environmental Protection Agency (EPA) has compiled a list of Disinfectants for Use against SARS-CoV-2 (COVID-19).
Doorway Management: Strategic opening and closing of doorways can prevent viral transmission. Opening high-flow doorways in hallways can reduce the number of high-touch surfaces in a facility, while closing the doors of individual office spaces can reduce cross-contamination of virus across office spaces. Doorway management approaches MUST consider operational security, facility security, safety, and privacy guidelines.
- Entrances/Exits: Hand sanitizer dispensers should be placed near entryways. Limiting the flow of traffic and personnel in and out of high traffic areas should be considered to reduce cross-contamination.
- Bathroom Entrances/Exits: Hand washing signs should be clearly posted. When possible, position trash cans inside bathrooms near the door to allow paper towel use and disposal for no-touch exit.
- Single occupancy: Best practice is to isolate personnel and patients in single occupancy to reduce the spread. Areas that were once open bays should be evaluated for ability to convert to single occupancy, if possible.
- Negative pressure rooms: The following are the best practices to limit the exposure of patients and staff: check with facilities management to ensure that the negative pressure rooms are functioning, evaluate for the possibility of adding negative pressure rooms as needed for the facility.
Note: Separate ventilation is important.
RESOURCES:
USCENTCOM Infection Prevention and Control Policy in a Deployed Setting (CCOP-02)
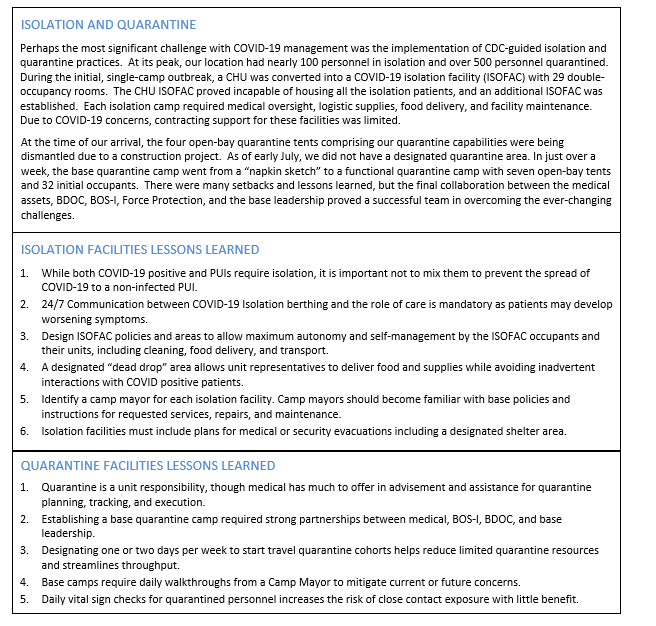
Isolation facilities (ISOFACs) will need to be established in accordance with best practice and other applicable guidance while taking into consideration the following issues:
- While both COVID-19 positive and PUIs require isolation, it is important not to mix them to prevent the spread of COVID-19 to a non-infected PUI.
- 24/7 communication between COVID-19 Isolation berthing and the medical personnel is mandatory as patients may develop worsening symptoms.
- Design ISOFAC policies and areas to allow maximum autonomy and self-management by the ISOFAC occupants and their units, including cleaning, food delivery, and transport.
- A designated “dead drop” area allows unit representatives to deliver food and supplies while avoiding inadvertent interactions with COVID positive patients.
- Identify a camp mayor for each isolation facility. Camp mayors should become familiar with base policies and instructions for requested services, repairs, and maintenance.
- Isolation facilities must include plans for medical or security evacuations including a designated shelter area.
ISOFACs are designed to allow outpatient recovery similar to a COVID positive patient recovering at home in CONUS. Unfortunately, most forward-deployed locations berth individuals in group berthing, this arrangement makes isolation difficult to achieve. While individual berthing with separated bathrooms is optimal, patient isolation cohorts may be the only option available. Isolation berthing should be designed to allow adequate comfort for multiple patients of varying symptom severity. Isolation areas should be well demarcated (e.g., “Isolation Area - No Unauthorized Access!”) and include posted guides on proper PPE procedures. Additionally, consider any medical evacuation routes in the event of worsening COVID-19 disease.
If possible, ISOFACs should include an entry anteroom that separates the outside from the isolation rooms and may include a designated “clean area” and “dirty area.” The clean area should be stocked with PPE and visual donning instructions. The “dirty area” should include a biohazard disposal bin and hand sanitizing station for doffing PPE.
A designated bunker should be pre-identified for the ISOFAC occupants in the event of an indirect fire. To mitigate transmission to non-isolated individuals, consider taping PPE bags to each door for patients to grab on their way to the bunker or other quick access methods.
Some ISOFACs may allow for individual/paired isolation (e.g. Containerized Housing Unit [CHU]), whereas others may require cohort isolation (e.g. tent). Subsequently, individual/paired isolation areas should be considered the preferred isolation site for females and individual cases. For unit outbreaks, cohort isolation may result in improved unit morale and accountability. Cohort isolation of confirmed cases can join pre-existing cohorts, whereas presumed positives (i.e. PUIs) should be isolated individually.
Medical personnel should conduct a daily sick call and should wear full PPE during encounters. Common symptoms may be immediately treated with over-the-counter medications; any individual with specific concerns should be evaluated. For worsening symptoms, consider obtaining vital signs and a NEWS score. Refer to Screening and Triage: Early Recognition of Patients with COVID-19 in the DoD Practice Management Guideline for current best practices.
Quarantine Facilities
Many sites have established a centralized base quarantine facility. However, it is important to realize that during a significant outbreak, the number of close contacts can quickly overwhelm any centralized facility. Therefore, units should have pre-established plans to quarantine close contacts within their living spaces. Quarantine is a command function, although medical issues that arise during quarantine should be referred to the appropriate medical unit.
Consider the following issues when establishing a comprehensive quarantine plan:
- Quarantine is a unit responsibility, though medical experts have much to offer in advisement and assistance for quarantine planning, tracking, and execution.
- Establishing a base quarantine camp requires strong partnerships between medical experts, Base Operating Support Integrator (BOS-I), Base Defense Operation Center (BDOC), and base leadership.
- Designating one or two days per week to initiate travel quarantine cohorts helps reduce limited quarantine resources and streamlines throughput.
- Base quarantine camps require daily walkthroughs from a Camp Mayor to mitigate current or future concerns. Daily vital sign checks for quarantined personnel increases the risk of close contact exposure with little benefit.
At a minimum, quarantine plans must include designated berthing areas, latrines, and showers for close contacts that are separated from the general populace. Meals should be delivered to quarantined individuals. Examples of unit quarantine plans include: 1) quarantining close contacts in their CHU rooms with a designated quarantine latrine, 2) moving close contacts into a designated quarantine tent that includes adjoining chemical latrines and portable shower units, and 3) deploying temporary fencing around an affected tent to designate it as a quarantined tent. Medical teams may provide guidance as units establish their quarantine plans and facilities.
Bases that serve as theater gateways experience a high volume of travel quarantine requirements. Quarantine cohorts must start and end their quarantine period as a group. However, it may prove infeasible to establish travel quarantine cohorts for each day’s arrivals. A base may choose to designate a fixed day(s) of the week for travel quarantines to begin. As an example, a base may begin a 14-day travel quarantine cohort every Tuesday. Incoming personnel who arrive Wednesday through Monday are placed into the upcoming quarantine cohort upon arrival; however, the 14-day quarantine period does not start until Tuesday. The entire cohort is then released to their respective units two weeks later. Individuals who do not abide by the quarantine order restart their 14-day quarantine along with all others in their cohort. This model requires three quarantine areas that rotate between the “fill” cohort, a cohort in their first quarantine week, and a cohort in their second quarantine week. Privacy dividers (e.g., central tent dividers) can allow males and females from the same cohort to share a cohort area.
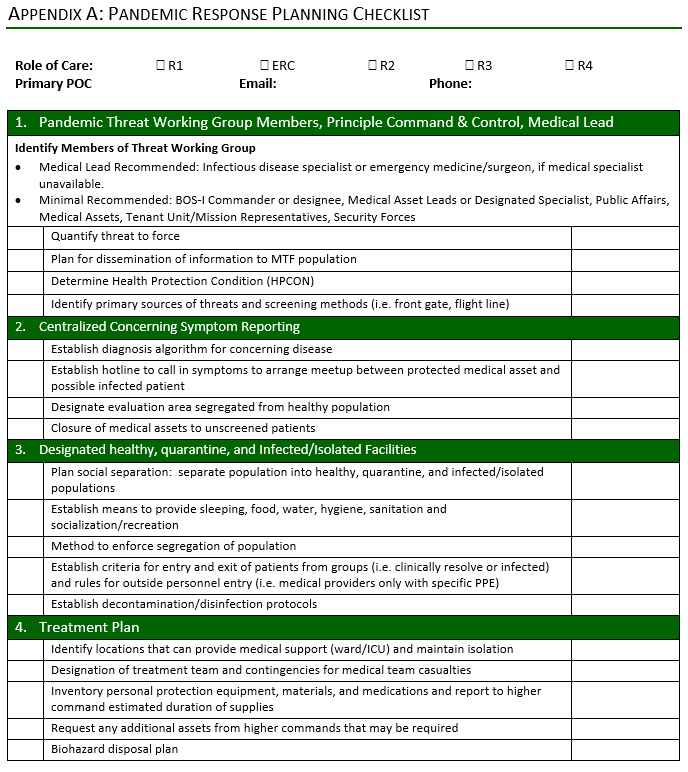
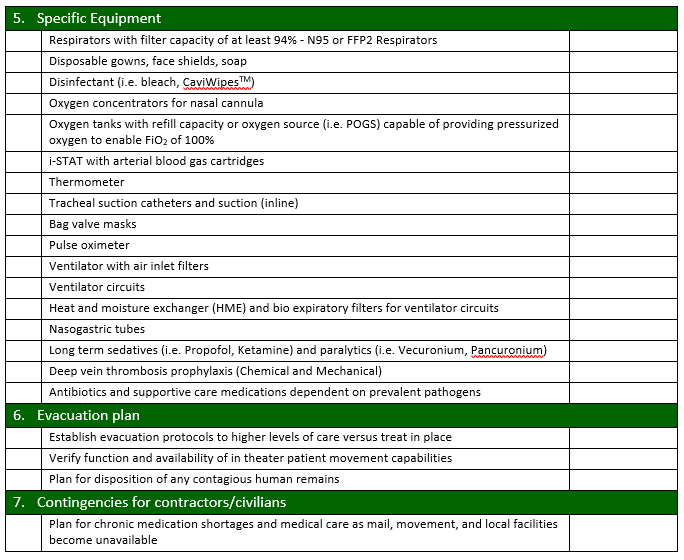
Units will investigate and proactively plan inpatient and outpatient surge capabilities within their existing resources. Special consideration should be given to preventing cross-infection of the patient population. A sample checklist to assist with surge capability planning at the role 1, 2, 3 level is at Appendix A.
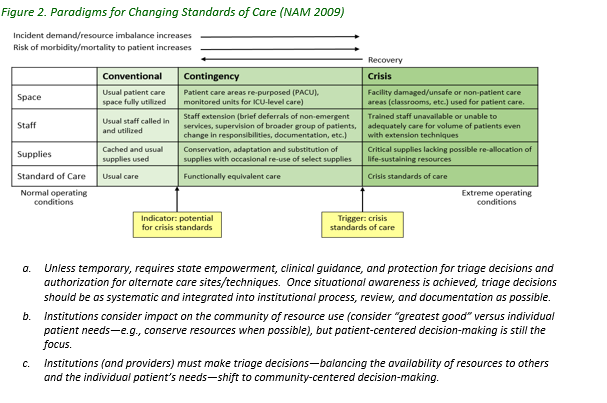
CSOC are guidelines that are applied when a pervasive or catastrophic disaster makes it impossible to achieve the usual standards of care.
The National Academies Press released an article from the National Academies of Sciences, Engineering and Medicine entitled, Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. This expert guide assists the provider in establishing a rationale for the implementation of crisis standards of care.
Additional assistance in developing and implementing this crisis standards of care can be accessed in the milBook through the following link: https://www.milsuite.mil/book/groups/covid-19-clinical-operations-group
There are limited resources for both the treatment and the diagnosis of COVID-19. Within the framework of responding to a global crisis, there must be evaluation and conservation of critical resources in terms of personnel, supplies and equipment. This section offers the resources for establishing a protocol for resource management with the focus on conservation. This is a broad approach and should be tailored to the resources of the facility for which the provider is managing.
RESOURCES:
USCENTCOM Policy for the Decontamination and Reuse of Filtering Facepiece Respirators (FFR) Such as the N95 (CAC required)
CDC Decontamination and Reuse of Filtering Facepiece Respirators
CDC Strategies to Optimize the Supply of PPE and Equipment
Table 1 published by the New England Journal of Medicine is a community standard consensus opinion of values.
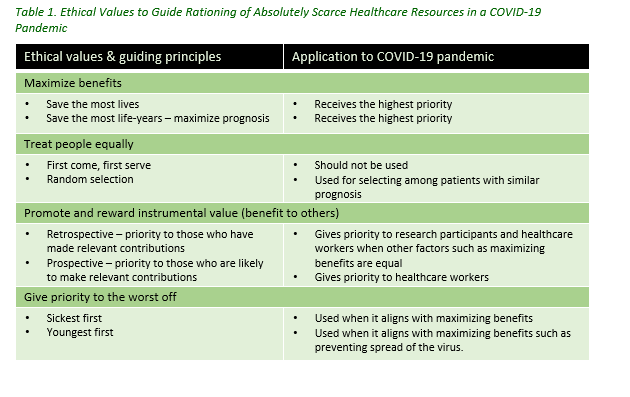
During a local, regional, national and global crisis, many decisions may require ethical considerations. These decisions are best managed in a multidisciplinary/multi-level command structure setting employing a good, better, best approach. See the following Resources listed.
RESOURCES:
DoD COVID-19 PMG v7.0, 3 March 2021:
- Ethics of Clinical Research during a Pandemic, p50
- Palliative Medicine during the COVID-19 Pandemic, p81-85
- Adjunctive Therapies: Treatment Protocols p49
- Planning And Preparation, p90-93
- Crisis Standards of Care: A Toolkit for indicators and Triggers, p138; Board on Health Sciences Policy; Institute of Medicine
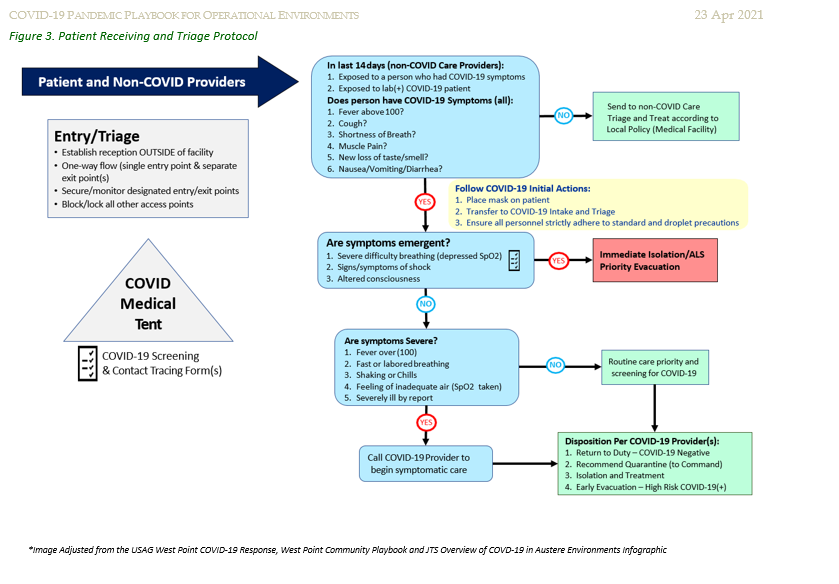
Medical triage is a familiar concept for all military medical personnel. The primary goal of saving as many lives as possible remains the same for pandemic disease triage. However, the operational concepts shift to the following main ideas:
- Identifying and cohorting infectious or potentially infectious persons as soon as possible.
- Identifying infected individuals who will most likely deteriorate rapidly/require prolonged advanced medical care to prioritize medical evacuation.
- During the triage process, treat patients as if they are possibly infected, and screen for appropriate need to continue to isolate patients based on symptoms.
RESOURCES:
Screening and Triage: Early Recognition of Patients with COVID-19, p11
Appendix B: Example Triage Protocols during COVID-19 Pandemic, p96
Management of COVID-19 in Austere Operational Environments CPG v3.0, 23 Apr 2021
Actions on Identification of a COVID-19 PUI, p5
Providing Medical Care to a COVID-19, p13
CDC Information on Contact Tracing and Epidemiologic Interviewing
Complete DD Form 3112, Personnel Accountability and Assessment Notification for Coronavirus Disease 2019 (COVID-19) Exposure, April 2020. Turn in DD Form 3112 to Public Health.
The following is an example of the patient intake and triage approach used by Task Force Medical 14:
- The trauma and COVID-19 screening and treatment locations were separated to minimize exposure.
- A speaker phone was placed outside the hospital entrance for direct access to the Patient Administration Department (PAD) line.
- Patients answered a series of questions to dictate their course.
- If COVID-19 was suspected and the patient was stable, they would wait to be assessed in the COVID-19 screening trailer located 50 meters from the hospital entrance.
- For patients deemed unstable, the evaluation would be conducted within the COVID-19 ICU.
- Pending the results of the provider’s assessment, the patient would either go into quarantine in the respective base location or get admitted to the COVID-19 portion of the medical footprint.
- Those that were able to be quarantined were evaluated at various intervals and provided meals by the hospital staff until release criteria was met.
Refer to Figure 3. Patient Receiving and Triage Protocol for more details about triage protocol.
Standard hospital infection prevention and control procedures will be implemented immediately in accordance with practice guidelines and best practice principles. Isolation (aka Transmission-Based Precautions) and Quarantine protocols are “step above” infection prevention and control measures employed in an epidemic/pandemic situation.
RESOURCES:
CDC Infection Control Guidelines & Guidance Library
Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care during the COVID-19 Pandemic
Infection Prevention and Control Non-Medical Considerations
Outside of medical settings, personnel must practice basic public health and infection prevention guidelines that focus on:
- Social Distancing
- Shelter-In-Place Activities
- Hygiene and General Protection Measures
Social Distancing is the practice of maintaining a minimum amount of separation between individuals and all other persons outside of their routine close contacts. Examples include roommates in barracks/quarters, family members in the same household, and teams that routinely experience unavoidable close contact in execution of daily duties (e.g., medical staff). For social distancing consider the following:
- Ensure that all personnel can maintain at least 6-ft spacing between themselves at all times.
- Ensure the lowest possible number of personnel in duty spaces (as needed to execute mission) and prevent (as much as possible) sharing of workspaces and equipment:
- Reduce the number of personnel in duty areas by instituting teleworking, day-on/off or week-on/off.
- Cohort all personnel into specific teams and ONLY persons from that team will work at the same time.
- Hand-overs will be done remotely or with a limited person(s) from the departing team.
- Each team cleans and disinfects the space, ESPECIALLY high touch surfaces prior to departing (See Hygiene and General Protection Measures).
Shelter-in-Place Restrictions require that all personnel limit their activity to quarters and their designated duty location (ONLY during their scheduled work period). This mandates NO social gathering or non-essential activities outside of personal areas AND closure of non-essential facilities (e.g., MWR, shoppettes). Essential activities/facilities include dining facilities (See Food Safety and Food Service section for more information duty activities as scheduled), medical care, and personal laundry.
Hygiene and General Protection Measures.
All personnel should maintain an elevated awareness of personal hygiene and routine cleaning practices that will prevent the spread of the virus including hand hygiene, routine wear of face coverings outside of personal areas, daily personal hygiene and grooming, cleaning/disinfection of high touch surfaces and common areas.
RESOURCES:
Non-Medical Infection Control, USCENTCOM Infection Prevention and Control Policy, p17-18. CAC required
CDC How to Protect Yourself and Others
CDC Cleaning and Disinfecting Your Facility
CDC Cleaning and Disinfecting Your Home
OSHA Guidance on Preparing Workplaces for COVID-19
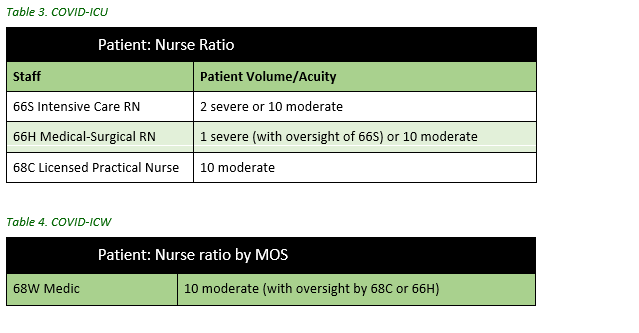
Outbreak response requires advanced staffing approaches to ensure safety and well-being of staff and patients, while limiting the spread of infectious disease. Facility managers should identify and assign essential personnel as per operational planning. Plans should identify tiered strategy planning and minimal risk approach. The tiered staffing strategy for pandemic (below) will be applied and tailored according to local resources and manning. Exact staffing plans and staffing ratios will depend on personnel, resources, and mission requirements. Additional considerations include:
- Designated and/or specialized COVID-19 care team separate from combat operations.
- Designated runners to ancillary services to reduce donning/doffing activities and protecting PPE supplies.
- Assignment and training of non-medical personnel to assist as runners, computer and administrative activities (e.g., transcribing notes for records, scanning/uploading patient files, etc.), and assisting with patient registration/screening (frontline).
- Work/rest cycles for prolonged management of potentially overwhelming numbers of critical care patients.
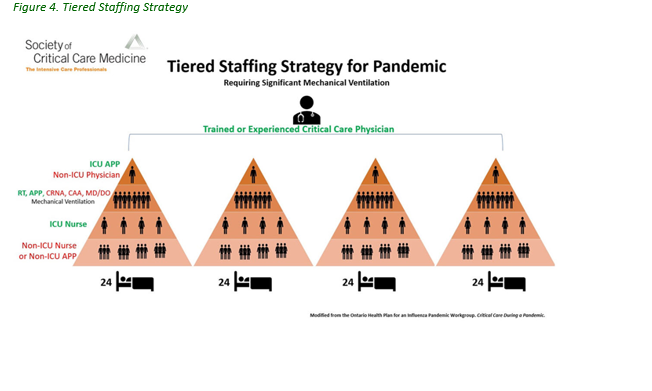
Case Example: Staffing Approach used by TF MED 14
A tiered approach assisted strategic staff management. Pandemic staffing ratios were used as a guideline, but modified based on tactical patient care/workload. Permitting unit skill sets, nursing personnel were categorized into COVID-19 and trauma teams. A minimum of two staff members were required on shift regardless of census and a critical care nurse for Rapid Response.
Cross-training/Up-training
All healthcare personnel should be up-trained and practice at the top of their licensure. All healthcare personnel should familiarize themselves with or review how to conduct certain critical activities (in case of personnel shortages):
- Use of critical care medications and ward stock.
- Daily preventative maintenance checks and services (PMCS) of critical equipment.
- Oxygen burn rate for patient usage and refill plan.
The following are recommended critical care topics for providers to review and drill to improve response and success in managing COVID-19 critical patients:
- Code Blue management of COVID-19 patient.
- Rapid Sequence Intubation roles of nursing staff.
- Ventilator management and Arterial Blood Gas (ABG) interpretation.
- Titration of critical care medications and side effects.
- PPE donning and doffing.
- Rapid response team parameters.
- Proning of a patient in an austere environment.
- Working knowledge of critical equipment (POGS, EDOCS).
- Unit specific standard operating procedures.
Units should conduct practice drills: PPE donning/doffing, patient procedures, transfers, proning, Code Blue, etc.
Leadership should consider cross-training non-medical personnel to assist clinical staff as appropriate and allowable. Non-medical personnel must perform Just-in-Time Training: DHA US-001 HIPAA and Privacy Act Training. CAC required.
Society of Critical Care Medicine provides free COVID-19 Resources for Non-ICU Clinicians. Topics include:
- Recognition and Assessment of the Seriously Ill Patient
- Critical Care for the Non-ICU Nurse
- Airway Management
- Airway Assessment and Management
- Diagnosis and Management of Acute Respiratory Failure
- Mechanical Ventilation
- Prone Positioning
- Diagnosis and Management of Shock
RESOURCES:
The Elsevier, COVID-19 Health Care Hub provides clinical toolkits, podcasts, expert opinions and many other tools for providers and staff in the COVID-19 response.
There are also resources for care of older adults and children. The web-based resources are free but require initial completion of a basic online form https://www.sccm.org/COVID19
The Defense Institute for Medical Operations (DIMO, www.dimo.af.mil) hosts the following courses:
- MASL D319329 - Medical Readiness Principles of Food Protection
- MASL D319328 - Malaria & Other Infectious Disease Threats
- MASL D319318 - Infection Control in Ebola & Pandemic Management
Individual risk assessment and fitness for duty for exposed healthcare workers should be determined with the support of COVID testing results, if available, and updated staff medical records. Updated CDC guidelines regarding healthcare workers can be found in the following resources list. In general, the following principles should be followed:
- All healthcare workers should engage in appropriate education, training and policies to comply with infection prevention and control.
- Any healthcare worker who develops fever or symptoms consistent with COVID-19 should immediately self-isolate and contact their established point of contact for testing.
- Per the CDC, “The utility of serologic testing to provide evidence of prior infection that would permit exclusion from quarantine has not been established and is not recommended for this purpose at this time.”
- Healthcare workers who are ill should not be involved in direct patient care.
Within the operational environment, health protection measures must be able to make allowances for mission-critical operational demands beyond the healthcare workers. Certain units, personnel, and functions are mission-critical and incapable of quarantining away from work for 14 days. To overcome this need, certain locations have established the concept of a “firewall” quarantine. While not an official CDC evolution, these firewall quarantines are designed to provide maximal protection from COVID-19 spread while allowing continued operations. It is modeled after the CDC’s recommendation for “Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to SARS-CoV-2.”
Firewall quarantine is a self-sustaining group of individuals exposed to COVID-19 that must continue to work to sustain mission-critical capabilities. For 14 days, these individuals quarantine and self-monitor for symptoms of COVID-19. They are only allowed in their designated workstation or berthing unit and must wear N95s whenever outside of berthing. Firewalled individuals are required to have separate basic life support (bathrooms, showers) from others who are not firewalled. They also use separate workstations from those who are not quarantined. Meals are delivered, and they are prohibited from visiting the barber, gym, PX, DFAC, etc., until the firewall quarantine completes. Any violations of the firewall quarantine will cause a restart of the 14-day quarantine for the whole firewall cohort and may subject the offender to UCMJ disciplinary actions. Examples of units that have successfully implemented firewall quarantine include healthcare facilities, base defense units, and command and control elements.
RESOURCES:
CDC Return to Work for Healthcare Personnel with Confirmed or Suspected COVID-19
Strategies to Mitigate Healthcare Personnel Staffing Shortages
Additional Training, Resources, and Tools are listed at Appendix B
Types Of Covid Tests
There are two broad types of COVID lab tests, distinguished by the method they use to detect infection:
- Viral Testing – Per CDC, any authorized assay for viral testing that detect either SARS-CoV-2 nucleic acid or antigen. Recommended to diagnose acute infection of both symptomatic and asymptomatic individuals, to guide contact tracing, treatment options, and isolation requirements. There are two major subtypes:
- a Antigen Testing - fast (<15 minutes) on-site testing that identifies COVID-specific structural components. Relatively inexpensive, but also less sensitive (higher chance of missing positive cases). Previously referred to as “Rapid Antigen Tests.” Renamed by the CDC in December 2020. May require Nucleic Acid Amplification Tests (NAAT) confirmatory testing under certain circumstances. Current FDA EUAs for antigen tests limits their use to symptomatic patients within a certain number of days of symptoms onsets. Special authorization was granted to the DoD by the FDA to use for serially screening asymptomatic individuals in certain circumstances.
- b NAATs - slower (1 hour - 2 days) in-lab testing that initiates an exponential multiplication of COVID nucleic acid. More expensive, but higher sensitivity (lower chance of missing positive cases) and specificity (lower chance of falsely identifying a true negative as positive) compared to antigen tests. Most common subtype is reverse transcription-polymerase chain reaction (RT-PCR) testing.
- Antibody Testing - in-lab test identifies the immune response to COVID (antibodies). The FDA has not authorized antibody tests to diagnose SARS-CoV-2. It is not approved for diagnosing current infection but may help determine whether an individual was previously infected. Issues with cross-reactivity to other similar virus antibodies. Commonly used for surveillance testing and epidemiologic studies.
RESOURCES:
Overview of Testing for SARS-CoV-2 (COVID-19)
Interim Guidance for Antigen Testing for SARS-CoV-2
Using Antibody Tests for COVID-19
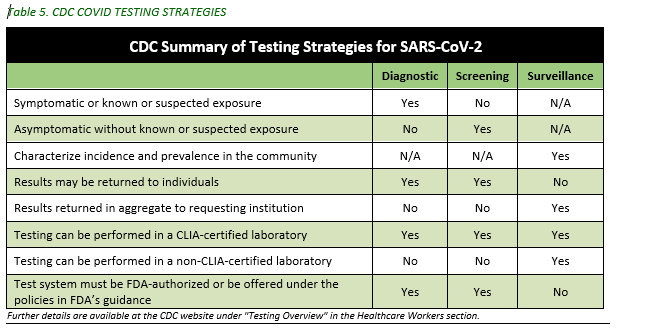
Covid Testing Strategies
There are also three broad categories for COVID testing strategies by the CDC:
- Diagnostic - used to identify current infection in symptomatic patients or asymptomatic close-contacts.
- Screening - used to identify infected persons who are asymptomatic and without known or suspected exposure. Screening testing is performed to identify persons who may be contagious so that measures can be taken to prevent further transmission.
- Surveillance - used to gain information at a population level with de-identified results returning in aggregate and not to the individual. It is intended to monitor community - or population-level outbreak of disease, or to characterize the incidence and prevalence of disease.
- Surveillance testing cannot be used for individual decision-making.
RESOURCES:
Overview of Testing for SARS-CoV-2 (COVID-19)
Frequently Asked Questions about Coronavirus (COVID-19) for Laboratories
Sample Pooling
When disease prevalence in an area is sufficiently low, certain Nucleic Acid Amplification Testing (NAAT) diagnostic testing systems are approved for sample pooling in order to save time and Class VIII materials. However, the combination of multiple specimens into one test dilutes the samples resulting in lower sensitivity. Theater lab officers should establish area-specific guidelines for pooling thresholds based on disease prevalence and specific equipment limitations. For example, the BioFire EUA (see the following resources list) includes three pages on approved pooling techniques. Lastly, pooling should only be executed at CLIP-certified laboratories.
The two most common NAAT systems in CENTCOM include the BioFire Diagnostic system and the GeneXpert family of diagnostic systems. At the time of this writing, the BioFire is approved for pooling samples; the GeneXpert systems are not approved for pooling. Pooled testing can be used for screening or diagnostic testing.
RESOURCES:
BioFire® COVID-19 Test Instructions for Use
DoD Testing Algorithms
Refer to current DoD Corona Virus Task Force COVID-19 Testing Protocols
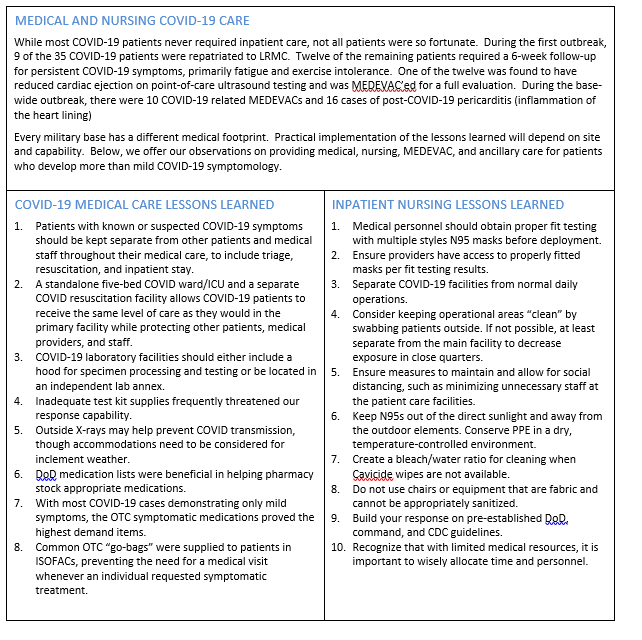
There is no cure for COVID-19. The treatment available now remains supportive care, which includes antipyretics, supplemental oxygen, and potentially mechanical ventilation. Medications currently used in the treatment of COVID-19 are off-label, are a part of research study protocols, or have been released by the FDA for Emergency Use Authorization.
COVID-19 has manifested primarily as a significant respiratory infection that can rapidly deteriorate into a severe pneumonitis, requiring supplemental oxygen and potentially mechanical ventilation. The severity seems to primarily affect the elderly population, and those with underlying medical comorbidities. However, this virus has also affected otherwise young healthy individuals. Providers must be aware and monitor all patients for potential rapid deterioration and intervene as soon as possible.
The DoD developed the DoD COVID-19 Practice Management Guidelines to assist providers throughout the DoD with comprehensive care for treatment and management of COVID-19.
With the decreased availability of staff and resources in the austere setting, a supplement to the DoD PMG for COVID-19 contains a section for considerations in the austere environment, under the same link immediately above.
Due to the global nature of this pandemic, as well as the infectivity of COVID-19, there are many special considerations when planning to evacuate patients from downrange. It is recognized that the DoD’s usual protocols and ability to evacuate patients has been severely limited. Patients may require treatment over a prolonged time (possibly several days) prior to evacuation to a higher echelon of care. It is a priority for the downrange provider to plan for longer than expected care. The DoD PMG for COVID-19 and the CPG for austere locations referenced previously, are useful tools. Additionally, the JTS prolonged field care guidelines, while not specific to COVID-19, are useful for prolonged field care and can be found within the following resources links.
RESOURCES:
JTS Nursing Interventions in Prolonged Field Care CPG, 22 Jul 2018
Discharging a patient from transmission-based precautions (TBP) AKA isolation should follow the CDC symptom based strategy. Patients can move through the various levels of care (mild outpatient self-care, moderate ward level care and severe ICU level care) but must remain in isolation and follow TBPs during this entire time.
For most adult patients with COVID-19 illness, isolation and precautions can be discontinued 10 days after symptom onset AND after resolution of fever for at least 24 hours, without the use of fever-reducing medication, AND with improvement of other symptoms.
Some adults with severe illness may produce replication-competent virus beyond 10 days that may warrant extending duration of isolation and precautions for up to 20 days after symptom onset.
For adults who never develop symptoms, isolation and other precautions can be discontinued 10 days after the date of their first positive RT-PCR test result.
RESOURCES:
Interim Guidance on Duration of Isolation and Precautions for Adults with COVID-19
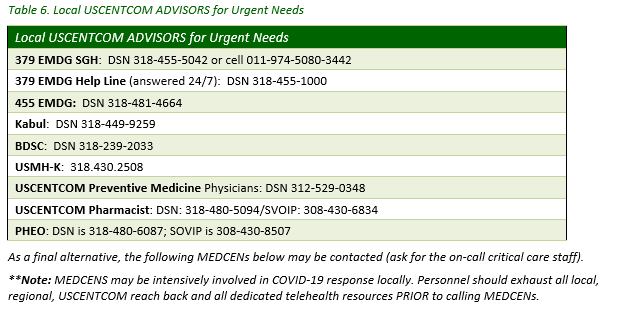
Listed below are emergency telehealth resources which forward-stationed medical teams/medics can use for assistance or clarification on any topics or concerns:
VITAL-T Program
Virtual Inspection and LINKUP in Theater (VITAL-T) provide “real time” virtual access to Quality and Safety (QS) expertise through Virtual Health (VH) capabilities for Infection Prevention and Control (IPC), Patient Safety (PS), and Medication Safety (MS).
Submit a Vital-T Consult in 2 Easy Steps
- Call with questions or to arrange a Virtual Consult or Service with the appropriate QS expert.
- Email: mailto:usarmy.jbsa.medcom.list.medcom-vitalt@mail.mil or 24-hour VITAL-T hotline: 210-307-0923
During the COVID-19 crisis, consult services could be conducted using any of the following approved means (the optimal means for connection will be individualized):
- Google Duo
- Skype
- FaceTime
- Adobe Connect
AD.VI.S.OR
Advanced Virtual Support for Operational Forces (AD.VI.S.OR ) program is specifically designed for operational virtual health support. Phone: 833-238-7756; Email: dod.advisor_office@mail.mil
Additionally, many Virtual Critical Care Consultation (VC3) service providers have deployed to austere settings before and can help work through the unique problems faced in austere settings.
DHA Infection Prevention and Control Tiger Team
The DHA Tiger Team is an alternative source for infection prevention and control reach-back, which is overwhelmed in the current situation. The team will review received questions on a daily basis and work to develop a response within 1-2 business days dha.ncr.clinic-support.list.ipc-group@mail.mil.
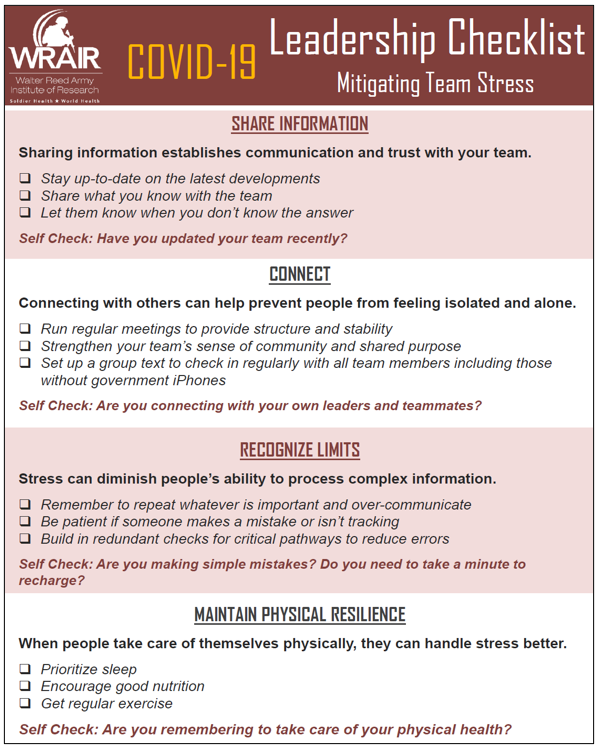
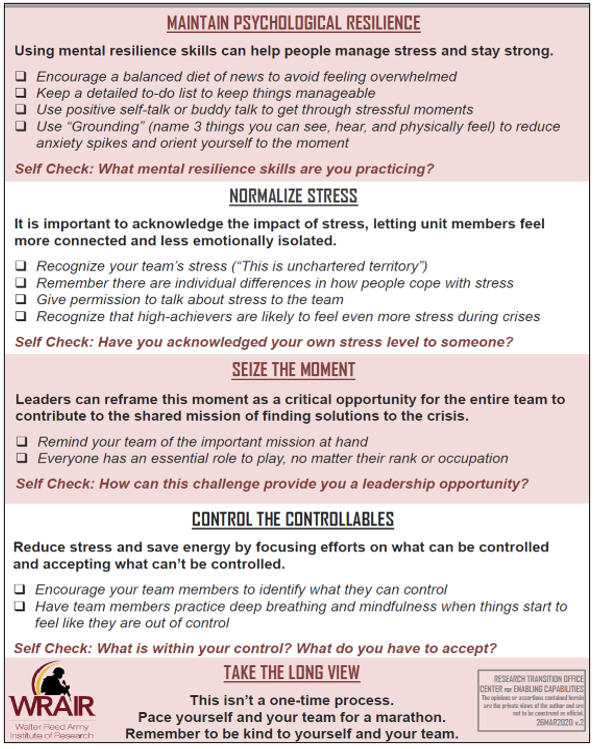
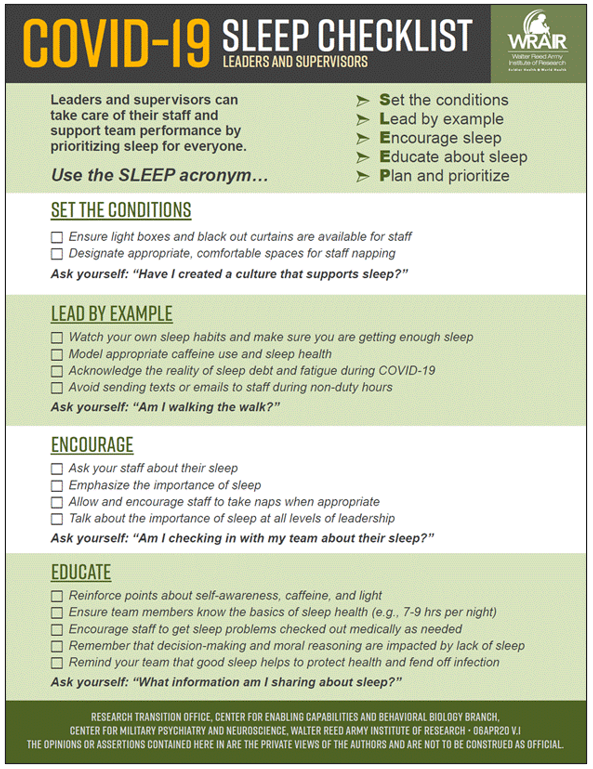
Leaders must consider the behavioral health and mental/physical resiliency of health providers and staff responding to an outbreak, as well as that of COVID-19 patients and the general population, who are experiencing major life-style changes and isolation. A number of tools and resources have been provided for leaders to respond to behavioral health concerns and improve resiliency. Forward stationed medics/medical teams are encouraged to reach back locally to Role 2/Role 3 facilities, where behavioral health resources may be stationed, utilize chaplain services, and telehealth resources to connect persons in need with help.
Special considerations for behavioral health during the COVID-19 pandemic include:
- Prolonged isolation of COVID-19 designated staff and patients.
- Disruption of non-duty activities and resiliency behaviors (e.g., physical activity, rest/relaxation).
- Risk for minimal work/rest cycles due to potentially overwhelming numbers.
- Moral stressors of triaging patients to receive care in the pandemic environment.
- Fear response for novel or unfamiliar risks/threats.
RESOURCES:
Behavioral Health and Wellness in Covid-19 Clinical Management (patients, providers) - DoD COVID-19 PMG v7.0, 3 March 2021 p93-96.
Resiliency/Well-Being – Stress and Coping, CDC Mental Health and Resiliency during COVID-19
Leadership checklist to mitigate team stress is located within Appendix C.
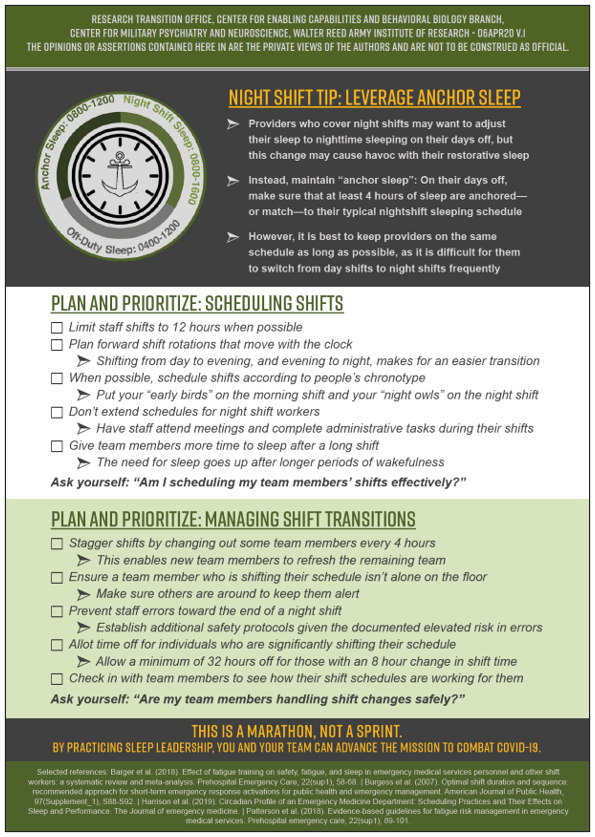
Leadership checklist to promote team sleep is located within Appendix D.
Navy Leader’s Guide for Managing Sailors in Distress – The purpose is to help Leaders recognize distress related behaviors, provide support to Sailors within the unit, and collaborate with Navy helping agencies to meet the needs of distressed individuals.
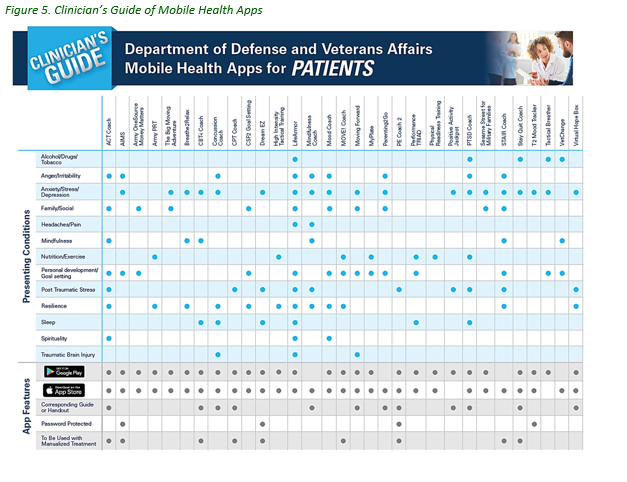
The DoD and VA offer the below mobile apps for mental health guidance.
Provider Resilience: Through psychoeducation and self-assessments, Provider Resilience gives frontline providers tools to keep themselves productive and emotionally healthy as they help our nation’s service members, veterans, and their families Apple and Android versions.
Psychological First Aid (PFA): PFA Mobile was designed to assist responders who provide psychological first aid (PFA) to adults, families, and children Apple and Android versions.
Other apps can be viewed by downloading the below brochure at https://health.mil/Reference-Center/Publications/2019/08/28/DoD-and-VA-Mobile-App-Clinicians-Guide. The Brochure does not provide links to the apps.
All U.S Military Service Members and U.S. Civilian personnel who die in an Operational Environment are under the medico-legal jurisdiction of Armed Forces Medical Examiner System (AFMES) in accordance with Title 10 U.S. Code 1471. If a death occurs, immediately notify AFMES at (202) 409-6811. All medical intervention should remain in place. Contact mortuary affairs for further guidance on the handling of the decedent. Secure clothing, personal protective gear, and medical/treatment records. These should accompany the decedent to mortuary affairs.
RESOURCE:
Ancillary service personnel will practice previously described infection prevention and COVID-19 medical management control measures.
Goals are to reduce the impact of exposure risks and preserve access to medications. Pharmacists will support ongoing clinical evaluation studies and treatment protocols for emerging therapeutics.
Once providers deem a diagnostic study necessary, take measures to minimize risk of cross contamination of equipment and environment. Equipment (including wheels) and X-ray cassettes shall be wiped down prior to entering and exiting patient care areas. Use disposable X-ray cassette protective sleeves or other type of similar barrier material for portable chest X-ray capability and equipment. Portable machines should be positioned so as to prevent contact with the patient whenever possible.
Appropriate PPE and infection control/prevention procedures to prevent blood borne pathogen and aerosol exposure will be employed. Patient screening may include nasopharyngeal swab specimens (most common) or tracheal aspirates from intubated patients.
RESOURCES:
Nasopharyngeal swab technique training video (7:19)
Management of COVID-19 in Austere Operational Environments v3.0, 23 Apr 2021, p9-10
Employed cleaning protocols should ensure adequate sanitization in all environments, including quarantine/isolation/patient care areas, as well as all workspaces and quarters. All non-dedicated, non-disposable medical equipment used for patient care should be cleaned and disinfected according to manufacturer’s instructions and facility policies.
- Routine Cleaning and Disinfection Procedures: Use cleaners and water to pre-clean surfaces prior to applying an EPA-registered, hospital-grade disinfectant to frequently touched surfaces or objects for appropriate contact times as indicated on the product’s label.
- High Touch Surfaces: In addition to standard environmental cleaning, employ routine cleaning of high-touch surfaces: tables, chair arm rests, doorknobs, light switches, countertops, handles, desks, phones, keyboards, mouse devices, toilets, faucets, sinks, etc.
- Bathroom Entrances/Exits: When possible, position trash cans inside bathrooms near the door to allow a no-touch exit. Hand washing signs should be placed in entryways.
RESOURCES:
FORCE HEALTH PROTECTION
Force Health Protection (FHP) assets which include the public health emergency officer (PHEO), public health, preventive medicine, and veterinary services are important stakeholders and subject matter experts on issues of infectious disease control (including zoonotic disease), sanitation, food protection and safety, and water systems protection and safety. Veterinary Services (VS) are equally important subject matter experts in animal medicine and husbandry, human-animal bond, and agricultural systems. Where available, FHP personnel should be consulted regarding these issues; there are now extensive Force Health Protection (FHP) Guidance documents published by the DoD available here: https://www.defense.gov/Explore/Spotlight/Coronavirus/Latest-DOD-Guidance/
A series of continually updated supplemental guidance documents outline the DoD position on all aspects of force health protection related to COVID-19 to include: testing, restriction of movement, diagnosis, recovery, travel restrictions, patient movement, non-pharmaceutical interventions (mask wear, social distancing, building occupancy restrictions, etc.), return to work criteria, and health protection conditions (HPCON). These FHP supplements are updated to include the evolving understanding about COVID-19 and changes in CDC and FDA recommendations and regulations. USCENTCOM policy is closely aligned with the DoD FHP documents but health care personnel must be familiar with both and should look to the link above regularly for updated information.
This information in this section is intended to supplement not supersede the USCENTCOM/Component and TRANSCOM policy and guidance. Any operational issues or challenges regarding FHP or the movement and care of authorized animals and animal-care personnel should be resolved through local, ARCENT, and USCENTCOM Command leadership.
Contact tracing is a critical part of COVID-19 mitigation, and must be supported by the command group. COVID Trace Team members will be required to complete training (see Appendix B: Additional Training and Resources). All positive cases will be contact traced and all individuals identified as a close contact will be placed in quarantine based on current USCENTCOM policy and DoD FHP guidance supplements. All confirmed cases will be contact traced and identified; close contacts will be placed in quarantine. Release from quarantine and isolation should follow current DoD and USCENTCOM policy but local commanders may impose more restrictive measures.
Field Sanitation and Isolation
In many cases, isolation facilities will need to be rapidly established that may require alternative waste and hygiene approaches to protect the uninfected general population (e.g. alternative showering facilities, pit latrines, bed cans). FHP assets should be consulted to ensure best possible practices are being implemented and that all safety and handling precautions are implemented.
RESOURCE:
Management of COVID-19 in Austere Operational Environments v3.0, 23 Apr 2021
Central Command Regulation 40-2 08 Nov 2017, Deployment Force Health Protection (SIPRNet)
DoDD 6200.04, Force Health Protection, Oct 2004
ATP 4-02.8, Force Health Protection, Mar 2016
Training Circular 4-02.3, Field Hygiene and Sanitation
Health Service Support Casualty Prevention for Expeditionary Operations, AFTTP 3-42.2, 2004
Food Safety and Food Service
There is still no evidence for concern that food and food packaging serves any role in transmission of COVID-19. Protection in dining facilities will focus on protection against direct human-to-human transmission and should include the following considerations.
- A la carte dining options (e.g., deli and sandwich stations, omelet stations) should be suspended during the pandemic.
- Fresh fruits and vegetables and deserts should not be presented in a salad bar format. These foods should be cleanly prepared and packaged in covered food containers.
- Meal lines and dining areas should consider social distancing. Seating should be placed in appropriate distances and/or limitations on capacity should be implemented. Consider outdoor dining options and take out approaches.
- Consider implementing servers – designated personnel that are screened for fever and symptoms at the start of each shift - instead of self-serve approaches or pre-plating or packaging meals to reduce contact during the serving process.
RESOURCE:
DoD Veterinary Services COVID-19 Resource Page Provides white papers, external links, situation reports and other operational guidance related to food safety and protection, FHP, and animal medicine/animal health during the COVID-19 pandemic.
Veterinary Care
Government owned animals (GOAs) and authorized privately owned animals (POAs) should continue to receive veterinary medical care in accordance with DoD and contact specific guidelines at local VS locations (veterinary treatment facility or similar). Any currently understood possibility of zoonotic transmission DOES NOT exceed the harm caused by not ensuring care for these animals. Elective procedures and veterinary medical care activities should be cancelled for the duration, but standards of care for public health and readiness should be maintained in accordance with applicable policy, health certificate requirements, and best practice guidelines (e.g. vaccination, emergency care, retail/distribution of medication and preventatives, etc.).
RESOURCES
DoD Veterinary Services COVID-19 Resource Page
American Veterinary Medical Association (AVMA) COVID-19 webpage
Animal to Human Transmission
The COVID-19 virus is known to have zoonotic origins, believed to originate at a live animal and wet market in Wuhan, China. It appears that in rare situations, COVID-19 infected persons can spread the virus to animals. The virus has been detected in felids (domestic cats, lions, tigers, snow leopards, and cougar), canids (domestic dogs), non-human primates (gorillas), and mustelids (ferrets, farmed mink and wild mink). It is unlikely that this virus will cause significant clinical disease in healthy domestic animals. There is no evidence to suggest domestic animals serve any significant epidemiological role in transmission of the virus to humans. Human-to-human transmission remains the primary source of transmission. However, given the possibility for zoonotic transmission of the COVID-19 virus, the following recommendations should be implemented:
- Commanders should strictly enforce USCENTCOM General Order (GO) 1C (paragraph 2.g) that prohibits the adoption of unauthorized pets or mascots of any kind on DoD installations. Exceptions to this policy include authorized GOAs, including military working dogs (MWDs) and DoD Contracted Working Dogs, and installations where personnel live off-base and are authorized POAs.
- It is not recommended to routinely test animals for COVID-19 using BioFire or any other testing platform. The CDC provides guidance on testing animals for COVID-19. The CCSG team and CENTCOM Command Veterinarian should be consulted PRIOR to any testing of animal patients for COVID-19.
RESOURCES
USCENTCOM General Order 1C (para. 2g), 21 May 2013
NASPHV Compendium of Measures to Prevent Disease Associated with Animals in Public Settings
CDC Evaluation for SARS CoV-2 Testing in Animals
DoD Guidance for Coronavirus Disease 2019 and Animals
Considerations for Animal Care Personnel
VS personnel should routinely implement and train local non-VS animal care personnel in the principles and standards of infection control outlined in the NASPHV Compendium of Measures to Prevent Disease Associated with Animals in Public Settings and applicable infection control policy and best practices. Elective veterinary visits and procedures should be cancelled through the pandemic. Animal care personnel should remain aware of current shortages and high demand of PPE for their human medical counterparts and practice prudent PPE implementation when treating animals, conducting laboratory procedures, and routine husbandry practices during the COVID-19 pandemic. The CDC makes recommendation on their website for PPE use when caring for animals. Working dog handlers that require isolation or quarantine should NOT conduct daily care for their dog. The Kennel Master, trainer, or other handlers should provide routine care for that dog until the assigned handler can return to duty.
RESOURCES:
NASPHV Compendium of Measures to Prevent Disease Associated with Animals in Public Settings
All disposable and non-durable medical supplies (including PPE) stock will be distributed and stocked IAW with pre-planning and role/location specific guidance.
Employ cleaning protocols to ensure adequate sanitization in all environments, including quarantine/isolation/ patient care areas, workspaces and quarters. All non-dedicated, non-disposable medical equipment used for patient care should be cleaned and disinfected according to existing location and USCENTCOCM specific infection control policies, manufacturer guidelines, and best practices.
The USCENTCOM Command Surgeon (CCSG) team is the main point of contact for this document at (813)-529-0345/0361/0362 (COMM/DSN) or centcom.macdill.centcom-hq.mbx.ccsg-clinops@mail.mil
LTC Fred Hauser and COL Vinh Tran are the USCENTCOM Public Health Emergency Office point of contacts and can be reached through the same organization mailbox (centcom.macdill.centcom-hq.mbx.ccsg-clinops@mail.mil)
AE Patient Classification...................................................................................................................... 1
Airborne Spread................................................................................................................................. 1
Ancillary Services.............................................................................................................................. 29
Antibody/Antigen............................................................................................................................... 2
Behavioral Health............................................................................................................................. 27
Cleaning, Disinfecting Households and Facilities................................................................................... 9
Contact Tracing ................................................................................................................................ 38
Critical Resource Conservation.......................................................................................................... 12
Command and Control........................................................................................................................ 4
Communications ................................................................................................................................ 5
Contact Spread................................................................................................................................... 2
Crisis Standards of Care....................................................................................................................... 3
Definitions ......................................................................................................................................... 1
Documentation ................................................................................................................................. 6
Droplet Spread................................................................................................................................... 2
Environmental Services/Housekeeping.............................................................................................. 29
Executive Summary............................................................................................................................ 1
Facilities Management ....................................................................................................................... 8
Field Sanitation and Isolation............................................................................................................. 31
Ethical Considerations....................................................................................................................... 13
Human Resources............................................................................................................................. 18
Hygiene, Social Distancing, Shelter in Place, and General Protection Measures.................................... 17
Infection Prevention and Control (IPC)............................................................................................... 25
Intermediate Care Ward (ICW)............................................................................................................ 2
Laboratory (Screening/Testing) ......................................................................................................... 29
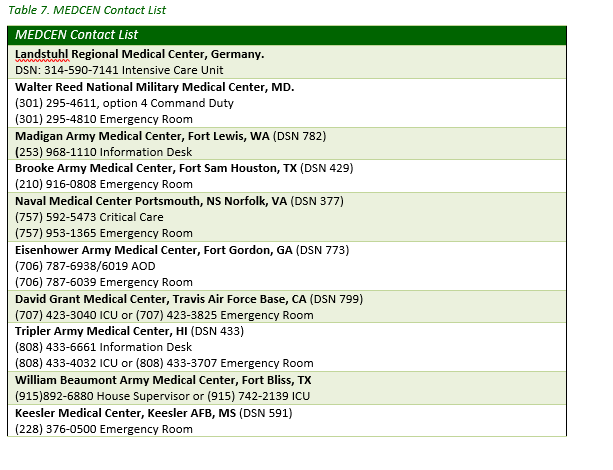
Medical Centers (MEDCENs), Contact Information.............................................................................. 26
Medical Management....................................................................................................................... 24
Mortuary Affairs............................................................................................................................... 28
Operational Planning ......................................................................................................................... 4
Pathogen.......................................................................................................................................... 29
Patient Under Investigation (PUI)........................................................................................................ 2
Performance Improvement ................................................................................................................ 6
Personal Protective Equipment (PPE) Considerations............................................................................ 8
Pharmacy......................................................................................................................................... 29
Quarantine Facilities......................................................................................................................... 10
Radiology......................................................................................................................................... 29
Resiliency/Well-Being....................................................................................................................... 27
Screening/Testing............................................................................................................................. 23
Skills Building/Training...................................................................................................................... 19
Staff (Patient: Staffing Ratios, Resilience/Well-Being).......................................................................... 18
Staff Surveillance and Staffing Decisions............................................................................................. 21
Supplies........................................................................................................................................... 33
Surge Capabilities............................................................................................................................. 11
Suspected, Confirmed Cases ............................................................................................................... 6
Telemedicine/VITAL-T/Points of Contact............................................................................................ 25
Transport........................................................................................................................................... 7
Triage/Security................................................................................................................................. 14
The following resources are available for rapid access and review in preparing for or responding to COVID-19 patients locally:
- Current COVID-19 Resources: Policy, Military-specific, Clinical, etc. will be posted in the DoD COVID-19 Clinical Operations Group site https://www.milsuite.mil/book/groups/covid-19-clinical-operations-group
- DoD Instruction for Public Health Emergency Management (PHEM) within the DoD. DoD6200.03 (28 Mar 2019) https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/620003p.pdf
- Joint Trauma System (JTS) Clinical Practice Guidelines (CPGs) https://jts.amedd.army.mil/index.cfm/PI_CPGs/cpgs
- The Elsevier, COVID-19 Health Care Hub. provides clinical toolkits, podcasts, expert opinions and many other tools for providers and staff in the COVID-19 response. https://elsevier.health/en-US/covid-19/home
- The Elsevier Engineering Resources for the COVID-19 response https://www.elsevier.com/connect/engineering-resources-for-the-covid-19-response
- Infection Prevention and Control Policy in a Deployed Setting and USCENTCOM Surgeon (CCSG) Clinical Operations SharePoint site (CAC Required) https://intelshare.intelink.gov/my.policy
- The US DoD Coronavirus Rumor Control should be used to clarify points of confusion and prevent decision making based on misinformation https://www.defense.gov/Explore/Spotlight/Coronavirus/Rumor-Control/fbclid/I/
- The Centers for Disease Control and Prevention, COVID-19 webpage https://www.cdc.gov/coronavirus/2019-ncov/index.html
- National Institute of Health, COVID19 webpage https://www.covid19treatmentguidelines.nih.gov/
- COVID-19: How to Conduct Contact Tracing, Health Information Products e-Catalog, Army Public Health Center https://ephc.amedd.army.mil/HIPECatalog/viewItem.aspx?id=1841
- COVID-19: Contact Tracing Toolkit, Health Information Products e-Catalog, Army Public Health Center https://phc.amedd.army.mil/topics/campaigns/covid19/Pages/Guidance-and-Alerts.aspx
- COVID-19 | Sustaining Operations: Roadmap to Coronavirus Disease Risk Reduction in Army Training Formations, COVID-19 | SUSTAINING OPERATIONS: Roadmap to Coronavirus Disease Risk Reduction in Army Training Formations, Health Information Products e-Catalog Army Public Health Center https://ephc.amedd.army.mil/HIPECatalog/viewItem.aspx?id=1834
Contributors (*Chapter Leads, †Main Editors)
LTC Jason B. Alisangco, MC, USA*
LT Emily A. Arnold, NC, USN*
HM3 Maxwell C. Basden, USN
HM2 James E. Bean, USN
CDR Robert C. Call, MC, USN*†
HM2 Tam V. Dang, USN
LT Timothy D. Dye, NC, USN
LT Amy L. Erdman, NC, USN
HM1 Antoine S. Giacometti, USN
LCDR Jason M. Hardwick, MC, USN*
HM2 Victor Isarraraz III, USN
CPT Rian N. Jockisch NC, USA
LCDR Arthur T. Johnson IV, MC, USN
LT Scott E. Krasovetz, MSC, USN
HM3 Sterling H. Magee, USN
LCDR Andrew E. Mancusi-Ungaro, MC, USN*
HM1 Christopher L. Moore, USN*
LT Nicole M. Pendry, NC, USN*
LCDR Kevin T. Petersen, MC, USN*†
CAPT Craig J. Randall, MC, USN*
HM2 Lucero E. Rocha, USN
HM2 Kareem S. Rouse, USN
CAPT Kristian E. Sanchack, MC, USN*
LTJG Jose E. Santos-Calderon, NC, USN
HMCS Johnny J. Stewart, USN*†
HM2 Michael L. Ward, Jr., USN
EXECUTIVE SUMMARY
INTRODUCTION
From June to November 2020, a forward location experienced four discrete COVID-19 outbreaks. Each outbreak revealed new improvement points, response flaws, and potential COVID-19 exposures. Consequently, the COVID-19 response posture for the location matured as a result of the outbreaks. With over 400 COVID-19 positive cases and more than 1,500 completed quarantines, this Executive Summary seeks to share our observations, narrative, setbacks, and lessons learned managing COVID-19 in an operational, forward-deployed setting. We approached this paper with honesty and transparency, as many of our worst days became our greatest teachers. We also quickly realized that sustained eradication of COVID-19 on our base would require a level of operational lockdown incompatible with operational requirements. Consequently, our end-goal became defined by our ability to mitigate COVID-19 from compromising the joint-coalition mission and not the number of COVID-19 cases or time between outbreaks.
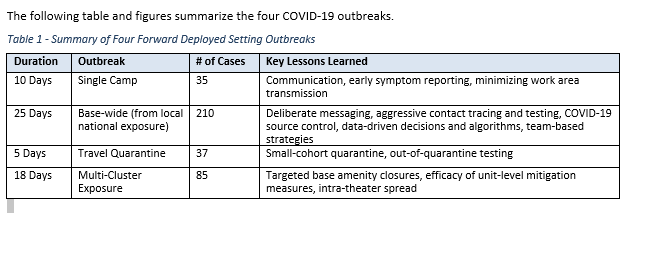
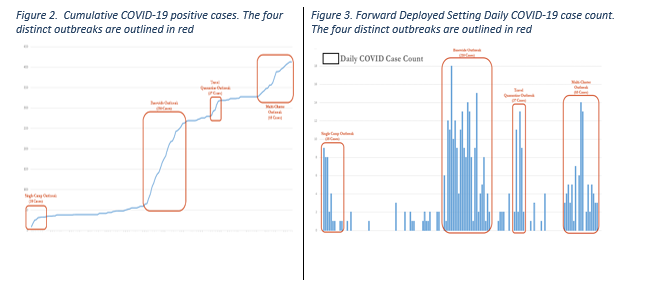
The subsequent chapters are deliberately detailed and intended for the reader seeking to develop and implement the described measures and strategies. A more concise summary is provided through this Executive Summary and the bulleted lessons learned at the beginning of each chapter.
The chapters are broken into four sections. The lessons learned from each chapter are included here in the Executive Summary. Further details can be found in the respective chapters. The first two chapters discuss the background and setting of COVID in the forward deployed setting. Chapters 3-7 focus on the fundamental principles of COVID-19 risk mitigation. The next two chapters, chapters 8-9, highlight events and lessons learned from our experiences building and maintaining isolation and quarantine facilities.
The final two chapters discuss austere medical and nursing COVID-19 care, as well as MEDEVAC considerations. Finally, the appendices are for supplemental usage and include the lessons learned report by unit surgeon from the initial, single-camp COVID-19 outbreak.
FUNDAMENTAL PRINCIPLES OF COVID-19 RISK MITIGATION
Bluntly stated, our location was not adequately prepared for the COVID-19 outbreaks that began in June and escalated into late August and early September. While the initial, single-camp outbreak provided early observations and lessons learned, it may have contributed to a false sense of security that COVID-19 could be easily contained and controlled. The base-wide outbreak occurring in August quickly dispelled this belief. During the 25-day outbreak, our leadership discovered that it required a deliberate, multi-faceted strategy to prevent widespread infection. Specifically, we developed a COVID-19 risk mitigation plan built upon the following principles:
- Aggressive Contact Tracing and Testing
- Deliberate Messaging
- COVID-19 Source Control
- Data-Driven Algorithms and Decisions
- Team-Based Solutions
A comparison between the base-wide outbreak and the subsequent multi-cluster outbreak suggests the validity of our methods. The local national base-wide outbreak began with a single exposure point and spread across the base. Over 25 days, there were 210 positive cases from 23 different units. In contrast, the operational exposure outbreak had five independent exposure sources, yet only lasted 18 days and had 85 positive cases. Despite four additional “patient zeros,” the outbreak lasted seven days less with 60% fewer cases. Additionally, base amenity closures were significantly reduced during the multi-cluster outbreak. Lastly, two units with a minimalist COVID-19 mitigation posture proved responsible for 51 of the 85 positive cases. With stricter internal mitigation practices in these two units, it is estimated that 60% of the cases could have been avoided.