Module 5: Tactical Trauma Assessment
Joint Trauma System
Tactical Trauma Assessment
In this module, we will introduce you to the concept of a tactical trauma assessment, or TTA. It involves assessing injuries, prioritizing treatments, and coordinating the care of a combat casualty. The practical application of this information in the form of skill stations and trauma lanes will take place throughout the rest of the course. It will also be evaluated at the end of the course in your final assessment.
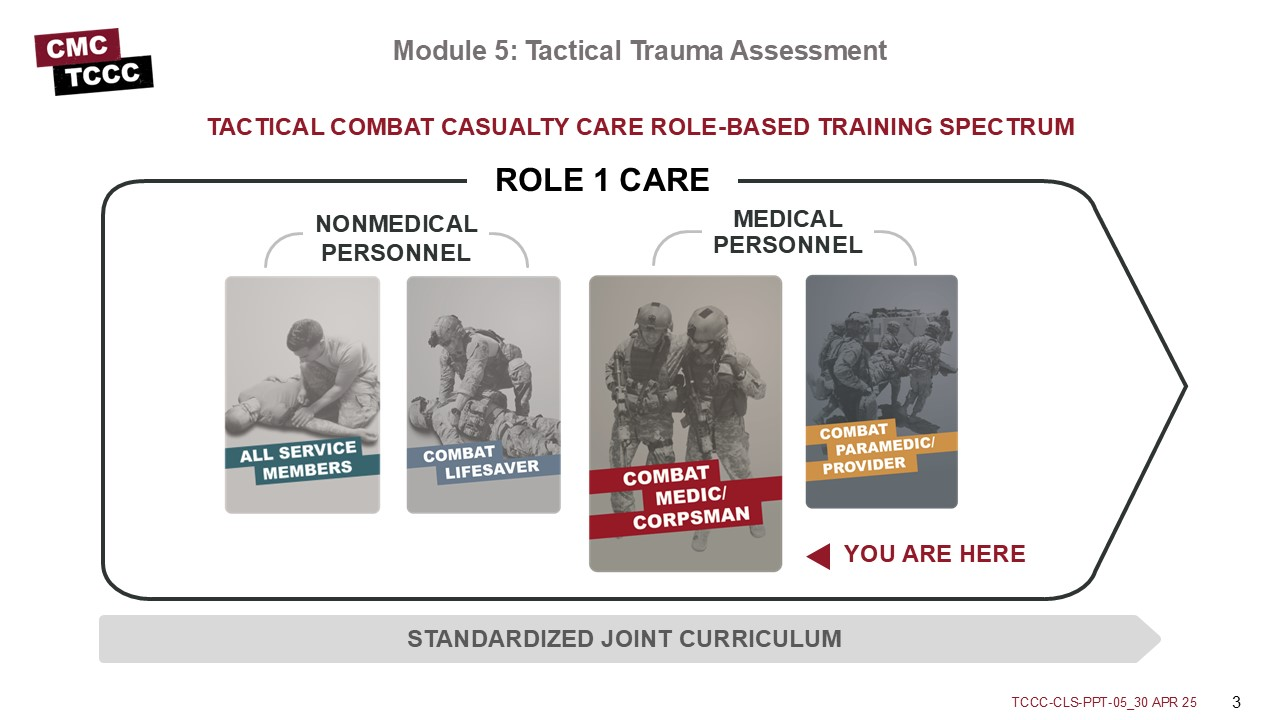
As a combat medic/corpsman, you are the first medical provider to care for the casualty and initiate more advanced treatments. As such, it is important that you understand the roles and responsibilities of the nonmedical personnel (ASM and CLS) who may be assessing casualties and providing care/assisting in care in the prehospital environment.
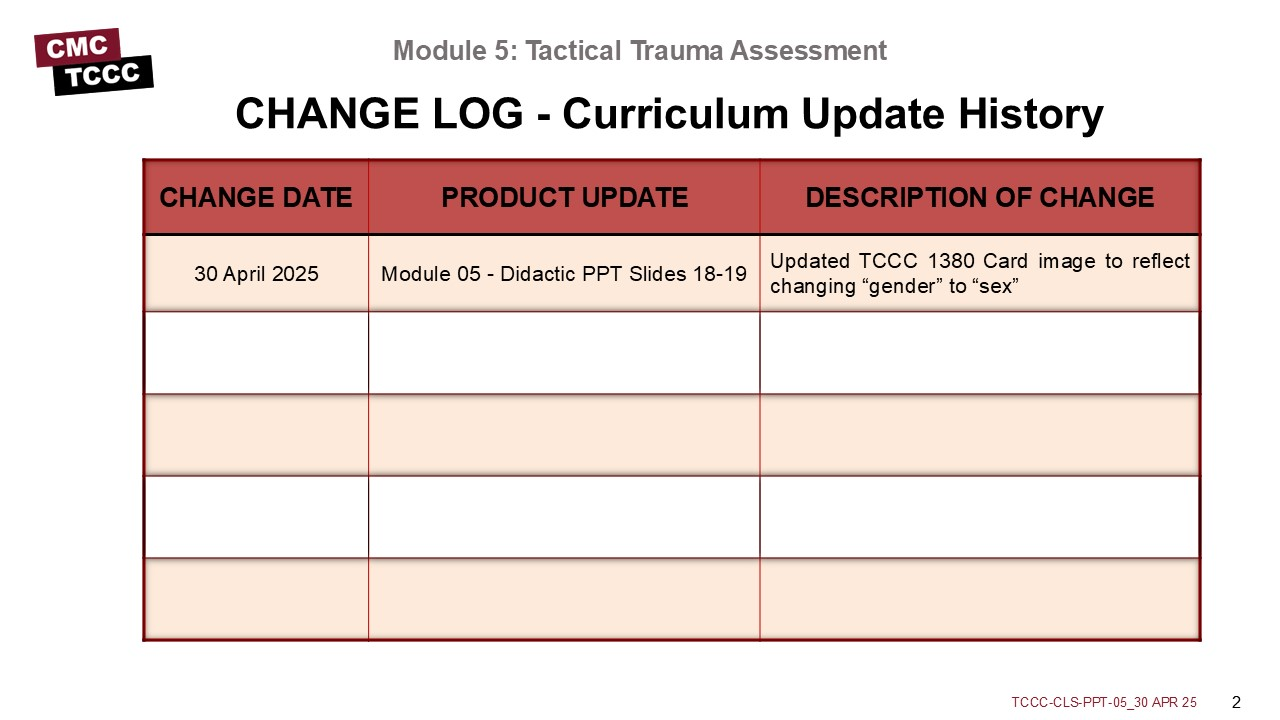
The Curriculum Change Log serves as a centralized reference to quickly track recent updates to training materials. It supports trainers by promoting clear communication, accountability, and alignment, helping stakeholders and learners understand what changes were made, why they were implemented, and when they occurred.
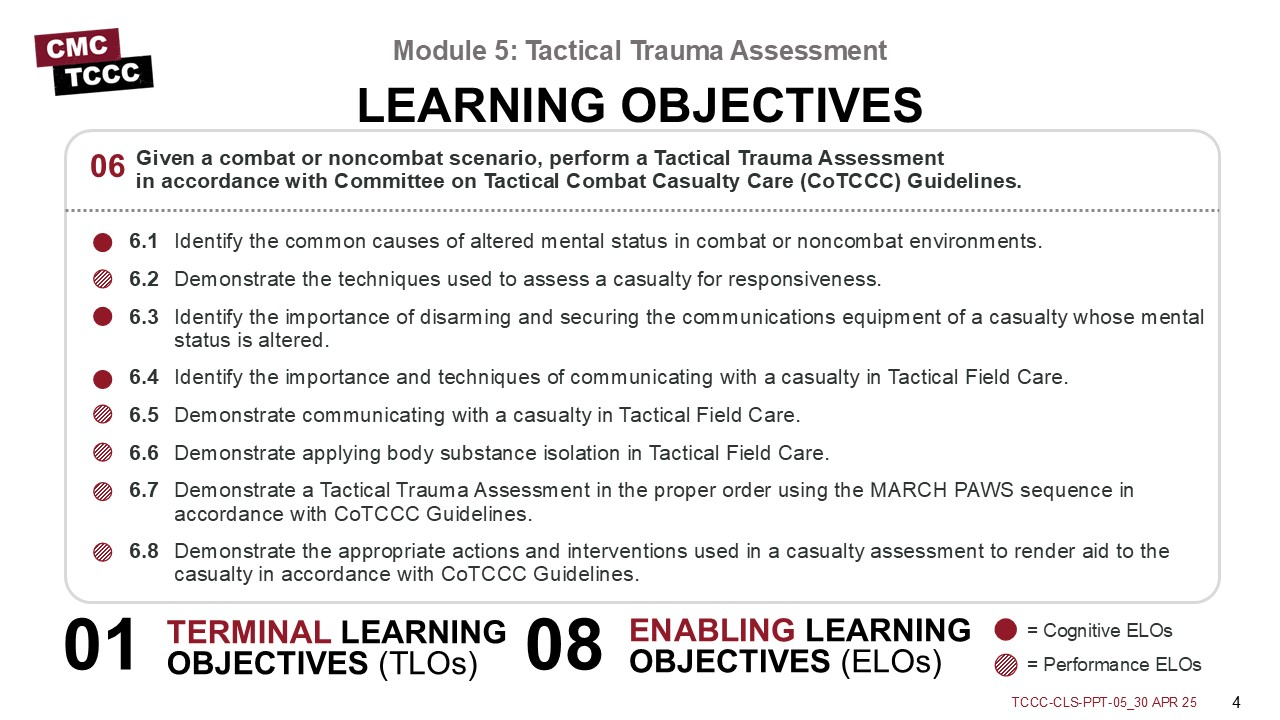
The Tactical Trauma Assessment module has three cognitive and five performance learning objectives.
The cognitive learning objectives are:
- Identify common causes of altered mental status.
- The importance of disarming and securing communications equipment from casualties with altered mental status.
- The importance of communicating with the casualty.
The performance learning objectives are:
- Demonstrate techniques for assessing a casualty’s mental status.
- Communicating with a casualty during Tactical Field Care.
- Using proper body substance isolation.
- Using the MARCH PAWS sequence to assess a combat casualty.
- Demonstrating the appropriate actions and interventions for a casualty based on that assessment.
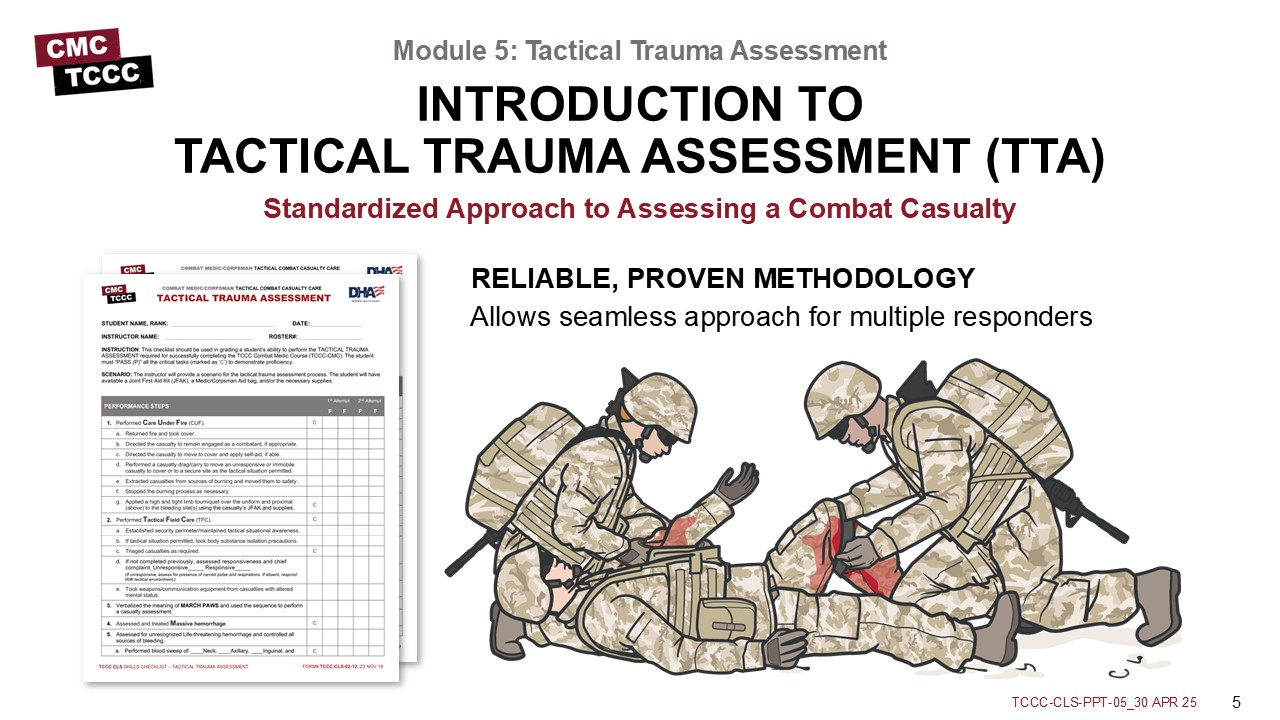
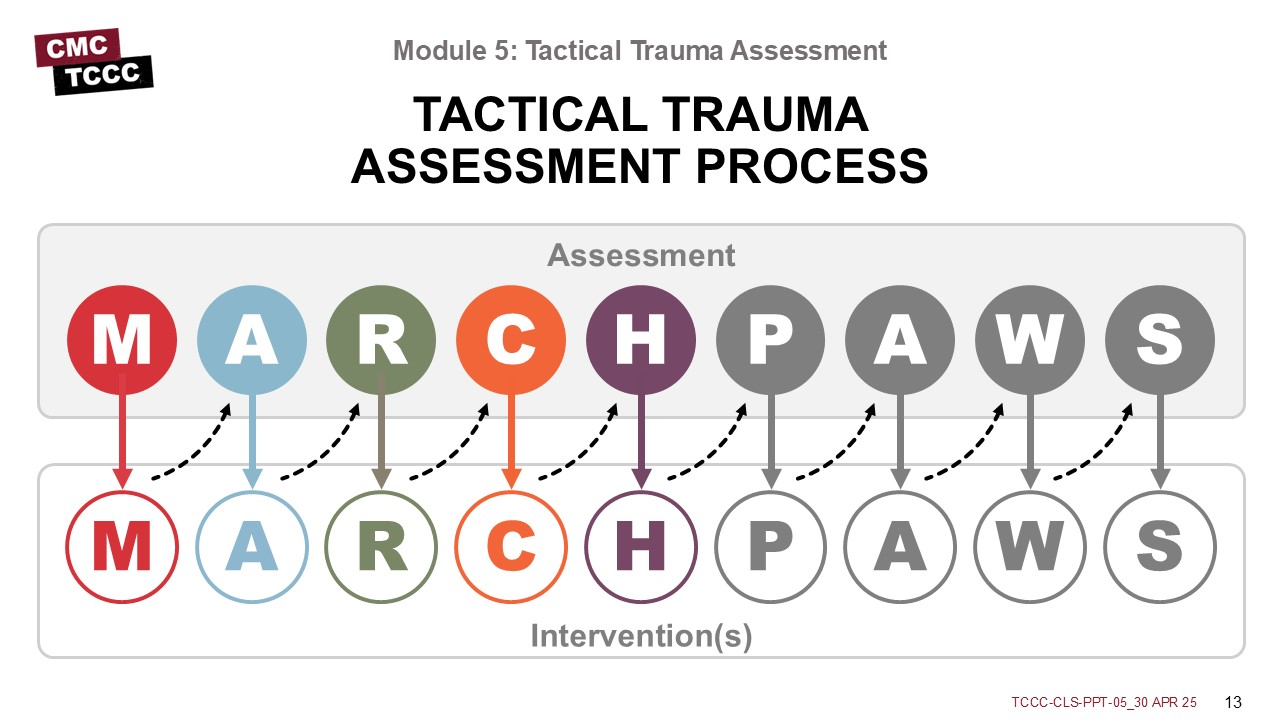
The TTA is a standardized approach for assessing a combat casualty. It reflects a prioritized algorithm or sequence of steps that has been proven to maximize the effectiveness of TCCC interventions in saving lives on the battlefield.
Also, with this standardized approach to assessment, responders can work together seamlessly, as each understands and can anticipate the next steps that should be taken in assessing and treating casualties throughout the continuum of care.
A few topics will be covered in more detail in this module that won’t be highlighted in subsequent modules. Identifying casualties with altered mental status is important, as this can significantly affect the TTA.
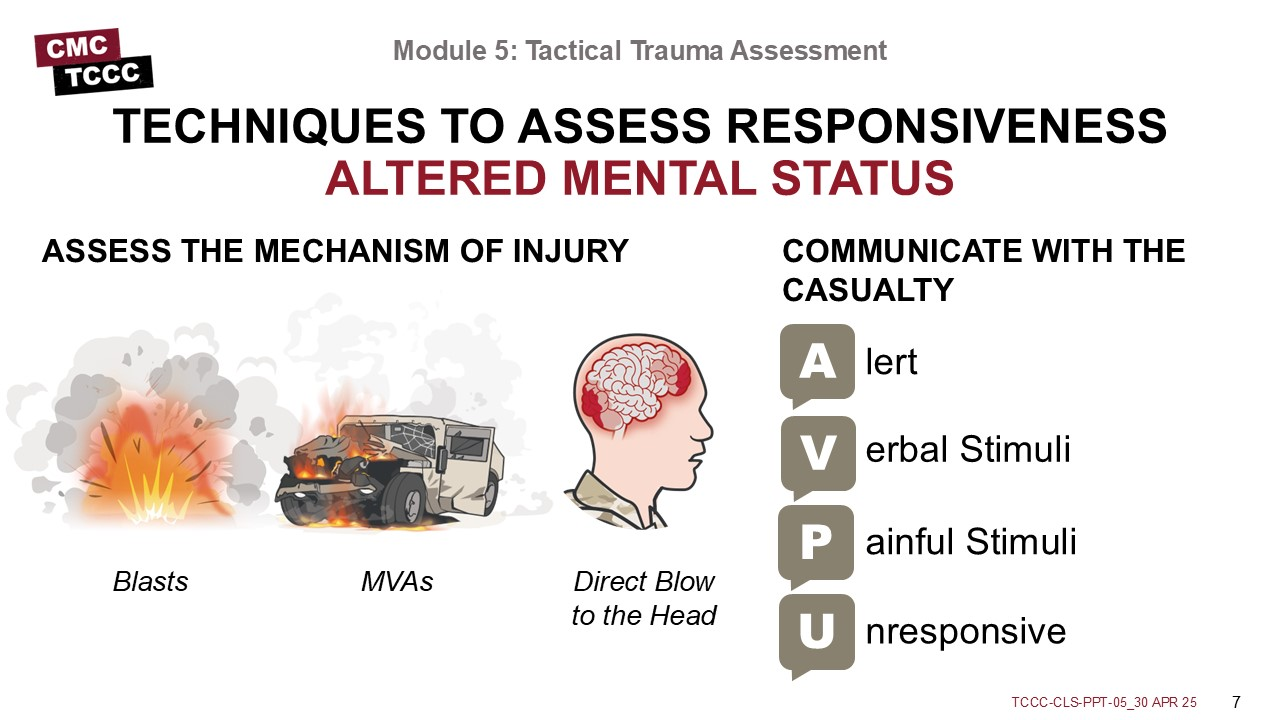
Altered mental status has several potential causes, such as metabolic, toxic, and infectious, but in the combat or trauma environment, the principal causes are traumatic brain injury, hypoxia, and hypovolemia from blood loss. Also, hypothermia, although not typically a primary cause, can exacerbate mental status changes.
Some pain medications can alter a casualty’s mental status, and this should be considered when assessing the casualty. Through determining the mechanism of injury and attempting to communicate with the casualty while assessing their verbal and nonverbal responses, you can determine if a casualty is not responding appropriately and exhibiting signs and symptoms of an altered mental status.
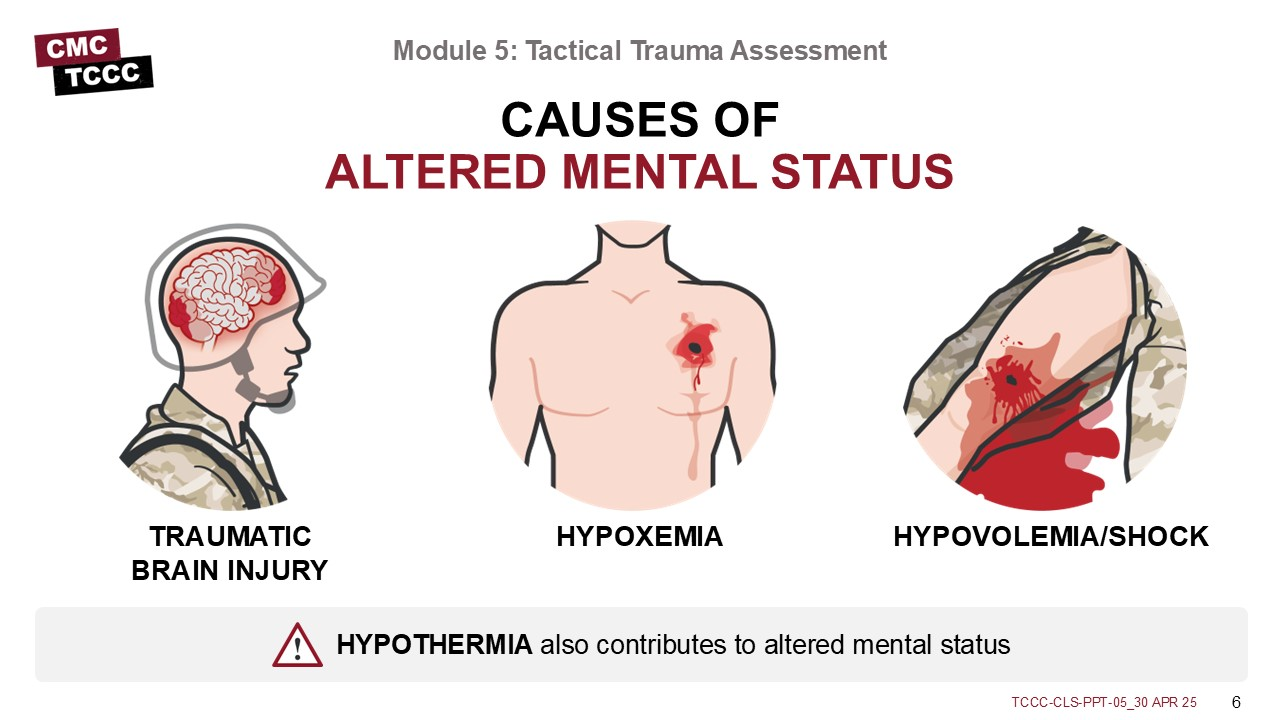
The mechanism of injury is often your first clue that a casualty has received injuries that might lead to an altered mental status. Specifically, exposure to blasts and significant impacts can lead to head injuries that are not always accompanied by obvious external signs. Of course, the presence of injuries that cause massive hemorrhage or altered respiratory status increase the likelihood of hypovolemia and/or hypoxia and should increase your suspicion that the casualty will have an altered mental status.
The initial rapid assessment of a casualty’s mental status comes from communicating with the casualty by asking them to follow commands and to answer questions. If the casualty is not responding appropriately (noticed by observing their verbal and nonverbal responses), this is a sign of an altered mental status. Later in the TTA, during the “H” of head injury evaluation, you will assess them using the AVPU technique. That involves assessing for responsiveness by validating whether the casualty is alert (the “A”), responds to your verbal commands appropriately (the “V”), responds to painful stimulation (the “P”), or is unresponsive (the “U”).
Casualties with an altered mental status often act (and react) inappropriately, and can even be a potential danger to themselves, first responders, and their unit, without being aware that their actions are improper.
Because of the possible threat this presents, responders must recognize when a casualty has an altered mental status and take steps to disarm the casualty and secure any communication equipment they may be carrying. Casualties are likely to resist this but will usually respond to reassurance that you are securing their equipment while you care for them and that their unit leadership will take responsibility for it.
In the prior module, communication with the casualty was also highlighted, along with some techniques to consider.
Communicating with the casualty is vitally important for several reasons. One is to help calm and reassure the casualty in what is likely the most stressful situation that they have ever experienced. If they are calmer, they will follow your instructions more closely, which may result in a better outcome. Also, as previously mentioned, communicating with the casualty allows you to assess their mental status and identify any changes over time that might lead you to an early reassessment of the casualty’s status.
As mentioned in the prior modules on the Principles of Tactical Field Care, you may have more than one casualty. You may need to triage casualties, direct the actions of other responders, and allocate your limited resources before beginning on an individual casualty assessment.
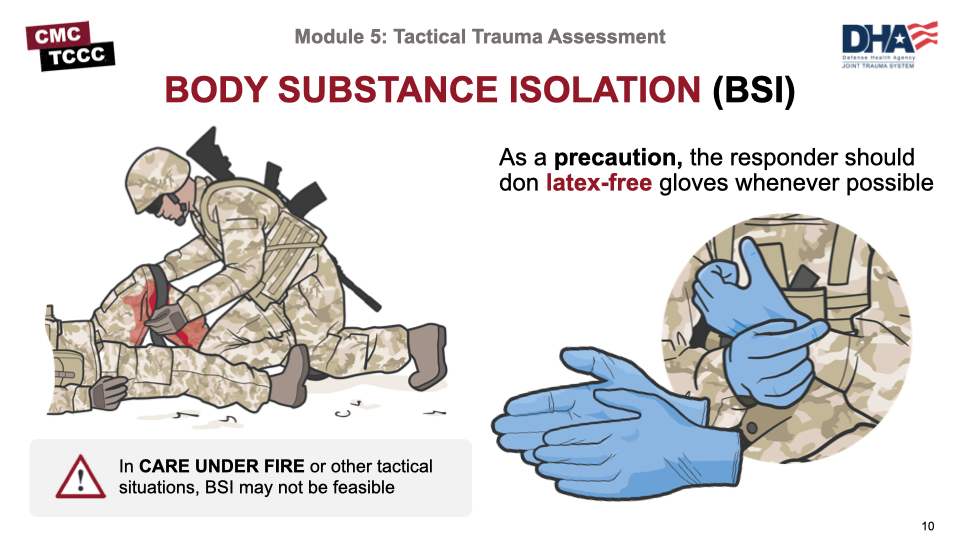
Body substance isolation (or BSI) is a situation-dependent consideration in TCCC. For example, in Care Under Fire, there is no time to worry about body substance isolation, although your tactical gloves do offer some level of protection. However, once in Tactical Field Care, whenever possible, responders should don latex-free gloves as a BSI precaution. Gloves are found in most equipment kits, including the JFAK, CLS bags, and combat medic aid bags.
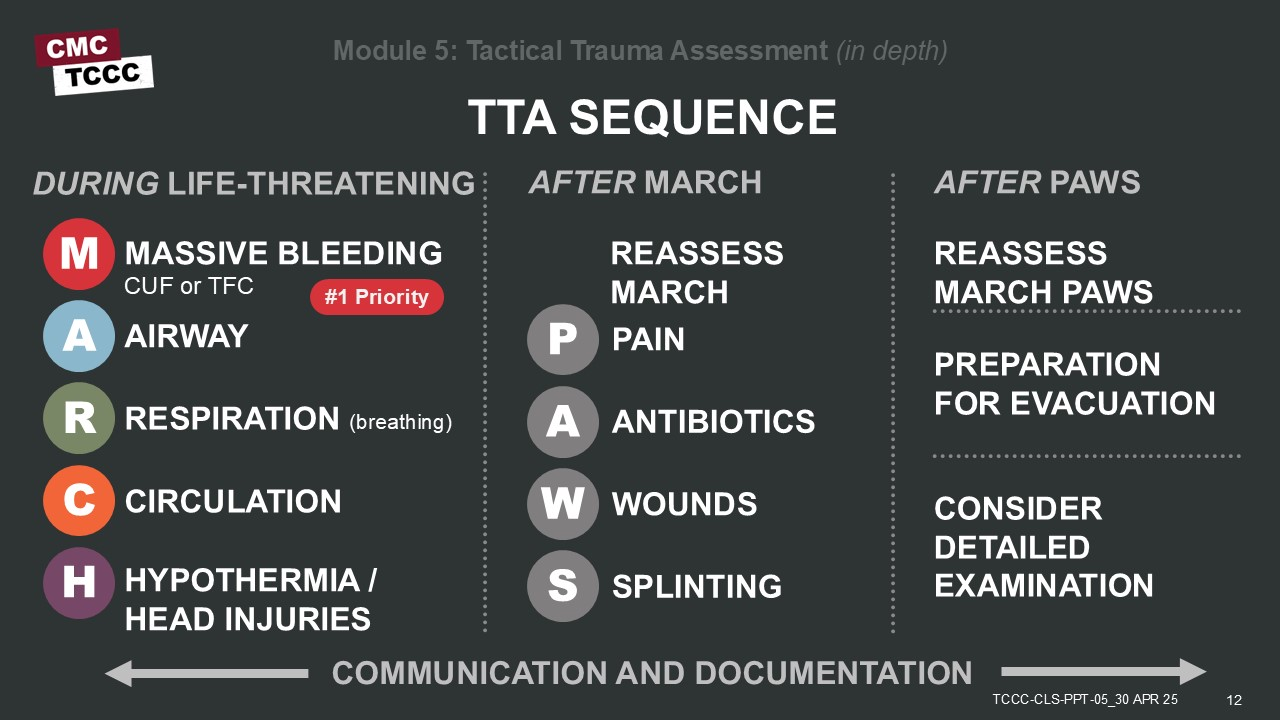
As you might expect, the TTA should begin by adhering to the MARCH PAWS sequence; understanding that massive hemorrhage assessment and treatment may begin in Care Under Fire while establishing fire superiority, extracting the casualty from burning vehicles or buildings, and moving them to safety, if appropriate. But most of the TTA occurs in Tactical Field Care, where further assessment and treatment following the full MARCH PAWS sequence can continue. Communication and documentation are key principles throughout the assessment.
As combat medics with additional skills and equipment, you may have time to perform a more detailed exam as part of a secondary assessment. The tactical trauma assessment can guide casualty care from point of injury through evacuation to higher-level care.
Throughout the rest of the course, we will cover the interventions and procedures of MARCH PAWS in more detail. Although we’ll take a moment to highlight some key concepts that apply throughout the TTA, we’ll defer discussions about the specific interventions until their corresponding module. For now, the focus should be more on the process than on the details of each procedure.
Remember that when performing an assessment, you will need to go back and forth from assessing the need for an intervention to performing a skill, and then return to assessing for the next potential injury. So, although we call this an assessment, the entire process is a combination of an assessment and a treatment plan being executed simultaneously.
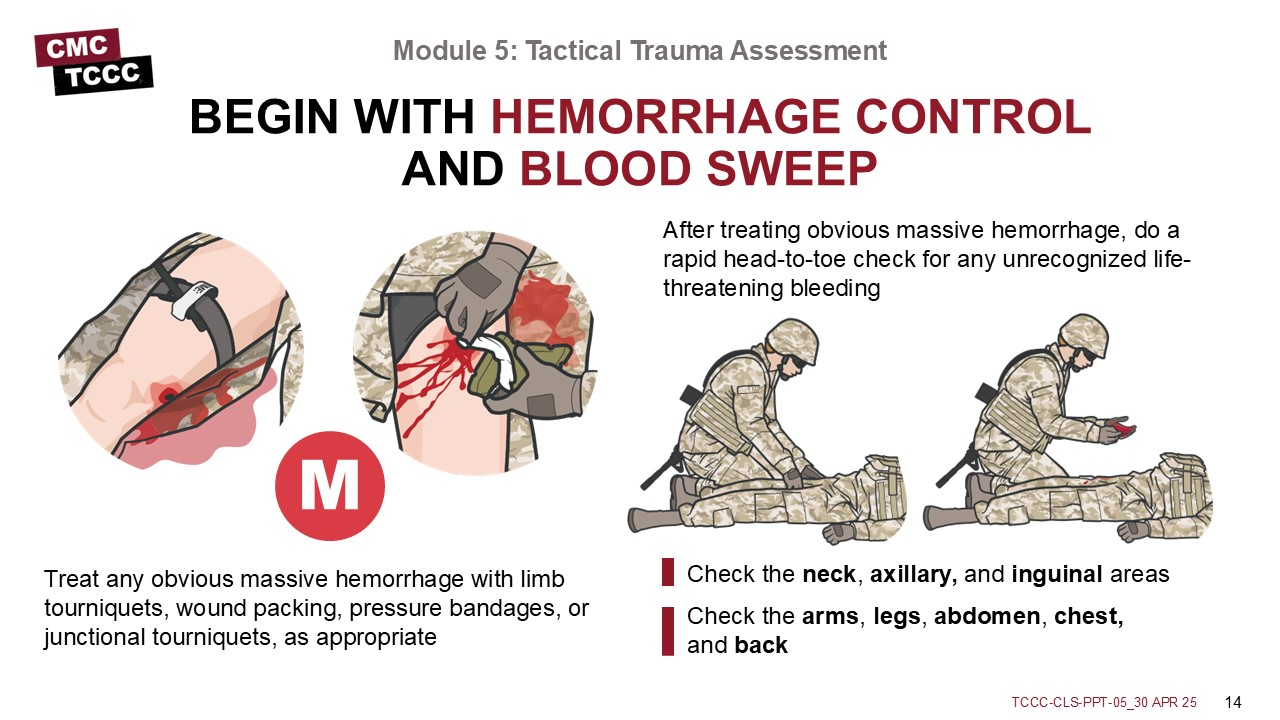
During the Care Under Fire phase conduct a visual blood sweep and apply CoTCCC-recommended limb tourniquet for hemorrhage that is anatomically amenable to tourniquet use.
In Tactical Field Care, immediately apply a tourniquet, hemostatic dressing, pressure dressing, or junctional tourniquet, as appropriate, to control massive hemorrhage. Part of the assessment at this point is to perform a head-to-toe check for any unrecognized life-threatening bleeding (called a blood sweep). This blood sweep is a visual and hands-on (palpating) inspection of the front and back of the casualty from head to toe, including the neck, axillae, and groin.
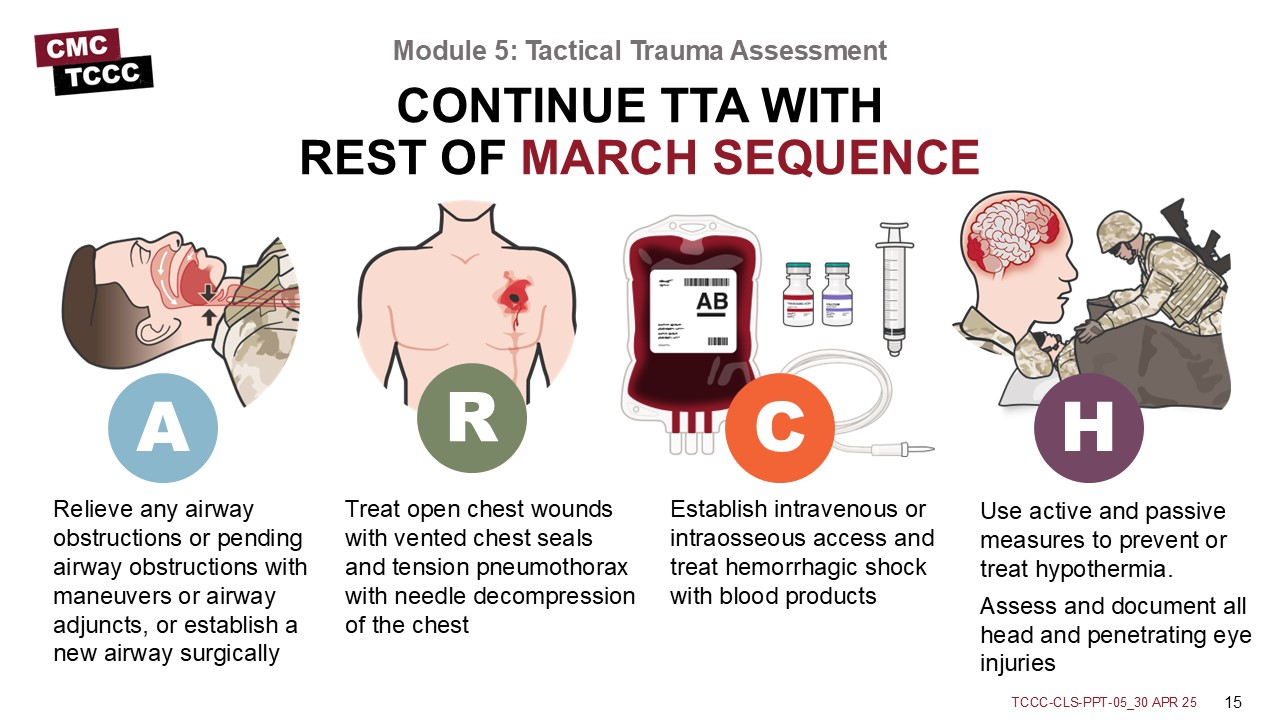
Once life-threatening hemorrhage has been addressed, the remaining MARCH sequence assessments and treatments can proceed. If you identify an airway obstruction, you should open it using either airway maneuvers or airway adjuncts. If those are not successful, you may need to establish an airway.
Sometimes an additional responder, such as a Combat Lifesaver, may be needed to help maintain an airway once re-established. Respiratory insufficiency may be from several different causes, and common trauma sources often respond to chest seals, or needle decompression(s) of the chest if a tension pneumothorax is present.
Circulation often focuses on applying a pelvic binder for cases of suspected pelvic fractures, reassessing prior tourniquet application, treating shock (when present), establishing intravenous or intraosseous access, and treating hemorrhagic shock with blood products.
Treat hypothermia with active and passive measures. Consider it a risk despite the ambient temperature of the environment. Assess, treat, and document all head and penetrating eye injuries.
These three efforts will help in the success in ensuring the best possible outcome for your casualty:
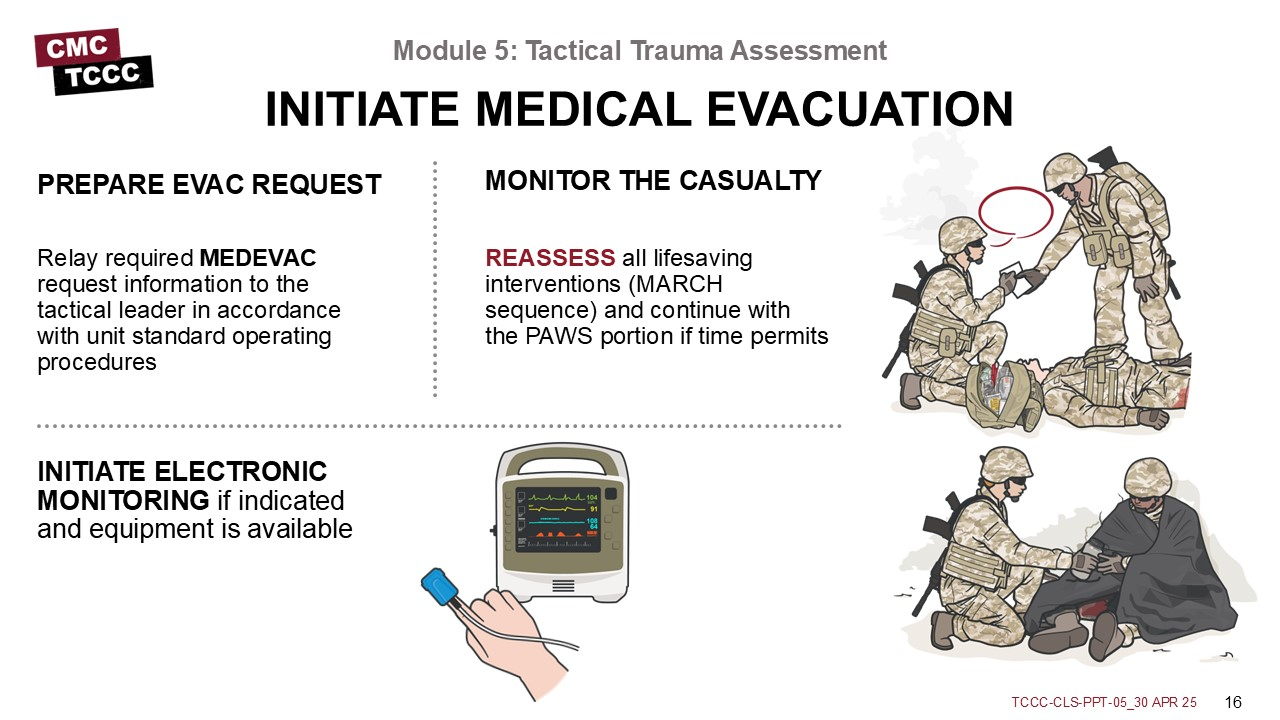
- Relay required MEDEVAC request information to the tactical leader in accordance with unit standard operating procedures
- REASSESS all lifesaving interventions (MARCH sequence) and continue with the PAWS portion if time permits
- INITIATE ELECTRONIC MONITORING if indicated and equipment is available
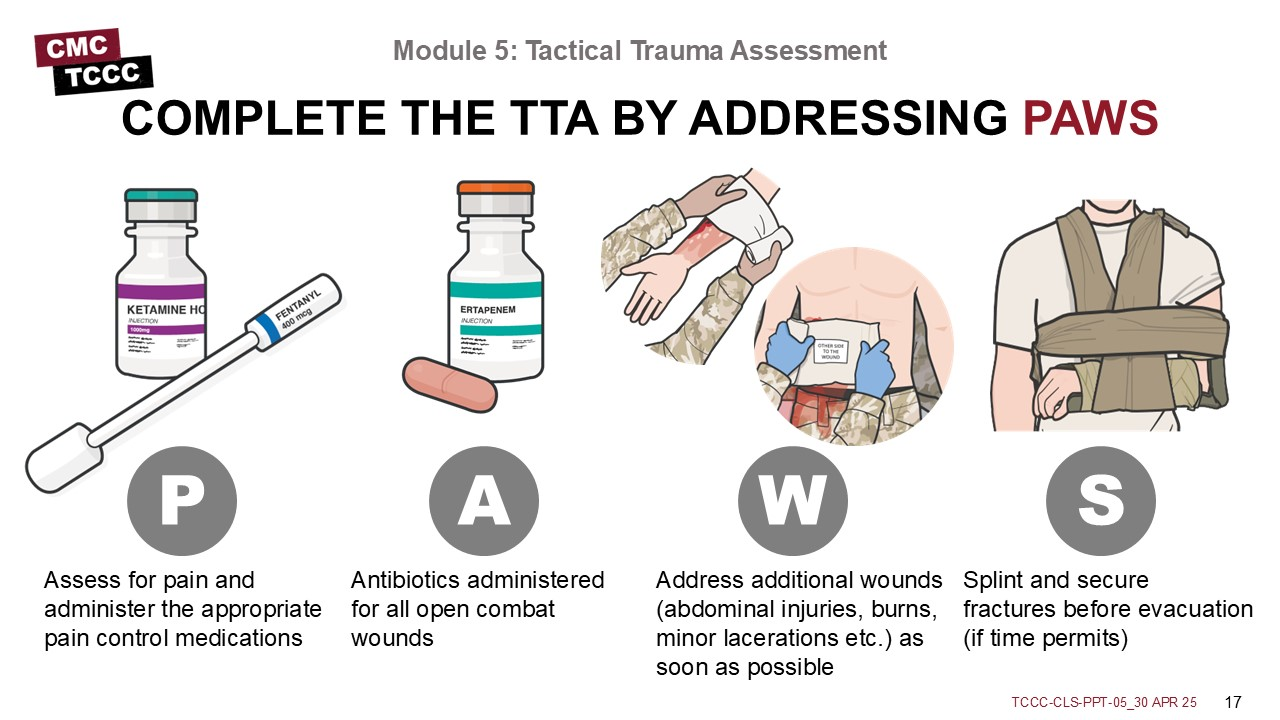
Once you have assessed the MARCH sequence and identified and treated any life-threatening issues, the next steps follow the PAWS sequence.Assess for pain and administer the appropriate pain control medications, keeping in mind the potential effect they may have on the casualty’s mental status. When appropriate, initiate antibiotic treatment. Several non-life-threatening wounds can result in significant long-term disability or deteriorate into life-threatening complications and need to be addressed as soon as possible. These include abdominal injuries, burns, or other soft tissue injuries. And fractures are common in the trauma environment and should be splinted and secured for evacuation.
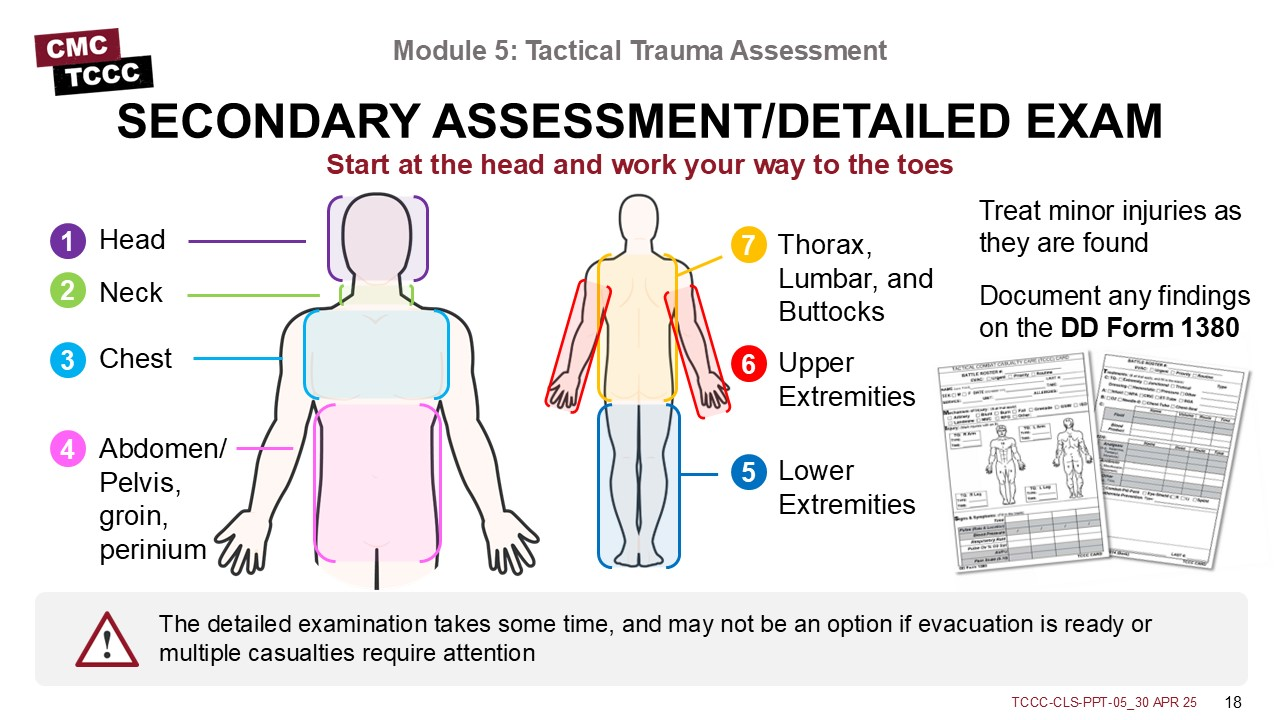
If time and tactical situation permit, perform a detailed examination and secondary assessment. This is most commonly done from head to toe to ensure that the examination is complete and nothing is overlooked. This includes the head, neck, chest, abdomen, pelvis, groin, perinium, lower extremities, upper extremities, posterior thorax, lumbar, and buttocks.
If you find any minor injuries, treat them as appropriate and document.
Preparing for evacuation involves several steps.
- Prepare the casualty to be evacuated (securing loose bandages, equipment, blankets, etc.) and place them on a litter appropriate for the type of evacuation.
- Prepare the site by directing the supporting personnel to establish security and a casualty movement process (often with litter-bearer teams), and by staging the casualties in the correct priority for evacuation.
- Prepare the incoming evacuation assets by communicating with them about the casualty status and anticipated requirements during the evacuation.
The Tactical Trauma Assessment is the process of assessing injuries, prioritizing treatments, and coordinating the care of a combat casualty.
Understanding common causes of and techniques to assess altered mental status is an important concept, especially since casualties whose mental status is altered must be disarmed and have their communication equipment removed.
Communicating with the casualty throughout the TTA is important to reassure them and maximize their response to any treatments rendered and to provide valuable insights into the casualty’s status over the course of their treatment.
When feasible, maintain body substance isolation.
The Tactical Trauma Assessment should follow the MARCH PAWS sequence to ensure a standardized approach that has been shown to yield the best outcomes for combat casualties. Time permitting, a more detailed physical exam can be performed before preparing the casualty for evacuation to the next level of medical care.
To close out this module, check your learning with the questions below (answers under the image).
Answers
In which phase of care is most of the Tactical Trauma Assessment performed?
Tactical Field Care (slide 5)
What pneumonic is used to prioritize care in the Tactical Trauma Assessment?
MARCH PAWS (slides 5 and 7)
Why is it important to assess the casualty’s mental status?
They may need to be disarmed and to have communications equipment removed. Following their mental status throughout the assessment may help responders identify changes in clinical status, leading to early casualty reassessment. (slides 10 and 11)
What is a blood sweep?
A blood sweep is a rapid visual and palpable head-to-toe check of the front and back of the casualty for any unrecognized life-threatening bleeding. (slide 14)