ACUTE RESUSCITATION
ASSESSMENT AND DOCUMENTATION/SUPPORT TOOLS
Calculate the patient’s initial burn size using the Rule of Nines (Appendix A). When wounds have been cleansed, re-calculate using the Lund-Browder chart (Appendix B and Appendix C). Superficial (1st degree) burns are NOT included in the estimation of burn size.
Superficial burns (1st degree) appear red, do not blister, and blanch readily. Partial-thickness burns (2nd degree) are moist and sensate, blister, and blanch. Full-thickness burns (3rd degree) appear leathery, dry, do not blanch, are insensate, and often contain thrombosed vessels.
If TBSA is 20% or greater, patients typically require acute fluid resuscitation for 24 to 48 hours postburn.
NOTE: In 10%-20% TBSA burns, maintenance IV fluids should be initiated, and urine output and other endpoints of resuscitation monitored closely. This is especially important in the setting of pre-existing dehydration, methamphetamine or alcohol intoxication, petroleum-based accelerants, concomitant electrical injury, or multisystem trauma as these may be associated with higher than anticipated fluid requirements.12,13
When performing fluid resuscitation, place a Urinary Catheter (with a calibrated urimeter chamber if available). Burns to the penis are not a contraindication to urinary catheter placement. Suprapubic bladder catheter placement is rarely required.
Hourly urine output (UOP) is the main index of resuscitation adequacy and assists with IV fluid adjustments. In adults, the goal is to achieve an hourly target UOP of 30-50 mL/hr (or 75-100 mL/hr for high-voltage electric injury).
Lactated Ringer’s (LR) or PlasmaLyte A are the preferred resuscitation fluids. Normal saline should be avoided, if possible, but can be used if absolutely necessary. ***Polytrauma patients with a source of hemorrhage should receive whole blood or balanced component therapy until hemorrhage is controlled and the patient is no longer coagulopathic. (Refer to JTS CPGs: Damage Control Resuscitation and Whole Blood Transfusion).
For adults, initiate IV fluid resuscitation using the Rule of 10s:10 mL/hr x %TBSA = initial fluid resuscitation rate.14
For patients weighing more than 80 kg, add 100 mL/hr to IV fluid rate for each 10 kg > 80 kg. Example: For a 100-kg patient with 50% TBSA, the initial rate is (10*50) + 200 = 700 mL/hr.
For children, 3 x TBSA x body weight in kg gives the volume for the first 24 hours. One half is programmed for delivery during the first 8 hours. Further guidance for pediatric management is provided below.
Example: a 30-kg child with 50% TBSA will need an estimated 30*50*3 = 4,500 mL during the first 24 hours. Half of this is 2,250 mL, to be given over the first 8 hours. Thus, the initial hourly rate is 2,250 mL/8 hrs = 281 mL/hr.
Use the Burn Resuscitation Worksheet (Appendix D) to assist initiation and documentation of fluid resuscitation.
If available, use the Burn Navigator for decision support.15 At the top of every hour, follow the prompts and enter the intake and UOP values. The device will provide isotonic fluid rate recommendations for the next hour. For guidance, see Appendix I: Burn Navigator.
Both under- and over-resuscitation can result in serious morbidity and mortality. Patients who receive over 250 mL/kg in the first 24 hours are at increased risk for severe complications including abdominal and extremity compartment syndromes.
In the absence of overt hypotension (MAP < 65 mmHg), avoid fluid boluses, as rapid changes in infusion rates contribute to edema. Instead, adjust IV fluid rates based on urine output (see below).
Colloid Rescue Recommendations
As early as 8-12 hours post-burn, if the following criteria are met, consider starting a colloid:
- Hourly IV fluid rate exceeds 1500 mL/hr.
- Projected 24-hour total fluid volume approaches 250 mL/kg.
- Other indications of significant hypovolemic shock despite IV fluid resuscitation.
- Evidence of compartment syndrome (such as bladder pressure > 20 mmHg).
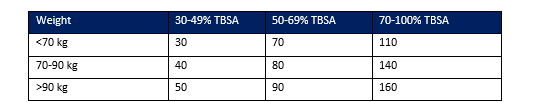
For adults: administer 5% albumin based on Table 1.
For children: give the colloid at the calculated maintenance rate (e.g., 4-2-1 rule), reducing the current isotonic infusion rate by an equal amount.
Continue the colloid infusion until the 48-hour mark. Typically, continue to adjust the crystalloid rate while keeping the colloid infusion constant.
Plasma is likely a superior resuscitation fluid because of protective effects on the endothelial glycocalyx. 18 Additionally burn shock is a plasma deficit, so early plasma resuscitation will result in less fluid shifts. For burns larger than 20% TBSA, consider utilizing plasma early if available, in combination with balanced crystalloid, using one of the following formulas:19,20
- Original Brooke Formula: estimated plasma dose for the first 24 hours is 0.5 ml/kg/TBSA. Estimated crystalloid dose is 1.5 ml/kg/TBSA. Example: 100 kg with 50% TBSA: initial plasma rate is 156 ml/hr; initial crystalloid rate is 468 ml/hr.
- Evans Formula: estimated plasma infusion dose for the first 24 hours is 1 mL/kg/TBSA. Estimated crystalloid dose is the same.
- When using these formulas, it is recommended to adjust the crystalloid dose hourly while keeping the plasma dose constant.
ALTERNATIVE STRATEGY: ENTERAL RESUSCITATION
Enteral resuscitation, also known as oral rehydration therapy, can be used in addition to or instead of IV fluids.21,22 (See Appendix G for the Oral Resuscitation Protocol.) Such fluids can be consumed orally (ideal route) by an awake and alert patient. They can also be administered via a nasogastric tube, orogastric tube, or by proctoclysis (enema). If given enterally, the resuscitation solution must be administered to the stomach and not directly to the small bowel due to large volumes required for resuscitation. Reasons for avoiding enteral resuscitation include the following:
- Abdominal injuries
- Gastrointestinal intolerance (vomiting)
- Pressor use >15mcg/min of norepinephrine (with or without vasopressin)
- Burns >40% TBSA (will likely need IV fluid augmentation).
Enteral resuscitation must include fluids that have salt, sugar, and are isotonic. Fluids like Gatorade will result in severe hyponatremia. Patients undergoing enteral resuscitation should be monitored for gastric residuals or vomiting. Enteral resuscitation through an NG tube/enteral tube must ensure that the fluid is gastric and not small bowel.
Titration and Goals of Fluid Resuscitation
Diligent fluid resuscitation in the first 24-48 hours prevents development of multiorgan failure in the setting of burn shock. This is why maintaining goals of resuscitation is essential in the care of a burn patient.
Urine Output:
1. 30-50 mL/hour in adults, or 0.5 to 1 ml/kg/hr in children
a. If UOP > 50 mL/hr, then decrease the IV fluid rate by 20%, wait two consecutive hours, and reassess.
b. If UOP < 30 mL/hr, then increase rate of IV fluids by 20%, wait two consecutive hours, and reassess.
2. 75-100 mL/hr for high-voltage electrical injury, or other conditions causing rhabdomyolysis
UOP may not be a reliable indicator of adequate resuscitation in some patients. Monitor hematocrit and lactate (and/or base deficit) as well. Successful resuscitation is indicated by resolution of hemoconcentration (e.g., hematocrit > 30%) and normalization of lactate.
Special considerations that increase fluid requirements in the first 24 hours:
- Hyperglycemia
- Illicit substance use
- Diuretics
- Alcohol
- Mechanical ventilation
- Additional trauma
- Preexisting dehydration
- Sedation or general anesthesia
Indicators of completed resuscitation:
- Patient follows commands
- Restoration of hemodynamics with minimal vasopressor requirement
- Adequate UOP of 30-50mL/hr
- Minimal fluid requirement
- Resolution of metabolic acidosis
- Hematocrit low to normal range (no further evidence of hemoconcentration)
If possible, measure bladder pressures every 4 hours in intubated patients if fluid resuscitation volumes during the first 24 hours are >200 mL/kg.5 Ensure the patient is in the supine position and follow the manufacturer's instructions for commercial kits; otherwise, use between 25 and 50 ml, being consistent in whatever volume is used, for serial measurements using a transducer located at the level of the symphysis pubis. Sustained bladder pressure >12 mmHg indicates early intra-abdominal hypertension and adjuncts such as colloid fluid should be considered for ongoing resuscitation. If the measured pressure is >20 mmHg, the patient should be fully sedated and paralyzed, and the measurement repeated. Persistent bladder pressures >20 mmHg may indicate abdominal compartment syndrome. (See Abdominal Compartment Syndrome below.)
PERSISTENT OLIGURIA AND HYPOTENSION
Clinically significant hypotension (mean arterial pressure, MAP < 65 mmHg) must be correlated with UOP and other indicators of resuscitation adequacy. Adequate end-organ perfusion as estimated by UOP 30-50 mL/hr generally requires a MAP > 65 mm Hg. Persistent oliguria and hypotension should trigger an assessment of the patient’s hemodynamic status and intravascular volume. Reassess for a possible missed injury or ongoing bleeding. Monitor intravascular fluid status using all available technologies. Consider early use of a colloid as discussed above as an adjunct.
If hypotension persists, use vasopressin 0.04 units/min (do not titrate) followed by norepinephrine (titrate 2-20 mcg/min) if needed. Epinephrine may be used as an additional vasopressor in severe shock proven to be non-hemorrhagic.
If intravascular volume appears adequate, STOP increasing IV fluid rate even if oliguria persists. Consider this patient hemodynamically optimized and that the oliguria likely results from an established renal insult. Expect and tolerate some degree of renal dysfunction in large burns. Continued increases in IV fluid administration, despite optimal hemodynamic parameters, will only result in “resuscitation morbidity,” which is often more detrimental than kidney injury.
If the patient exhibits catecholamine (vasopressor)-resistant shock, consider the following diagnoses:
- Missed injury and/or on-going blood loss.
- If pH < 7.20, adjust ventilator settings to target PCO2 30-35 mmHg. If, despite optimal ventilation, patient still has a pH < 7.2, consider administration of sodium bicarbonate.
- Adrenal insufficiency.6
- Consider empirically administering calcium chloride (8-16 mg/kg IV) for refractory hypotension, especially in patients who have received a blood transfusion. If able to measure levels, maintain ionized calcium >/= 1.2 mmol/L.