Module 6: Massive Hemorrhage Control
Joint Trauma System
Massive Hemorrhage Control
During this module, we will introduce you to the techniques for identifying and controlling massive hemorrhage. The practical application of this information and the techniques in the form of skills stations and trauma lanes will take place throughout the remainder of the course, and will be evaluated at the end of the course during your final assessment.
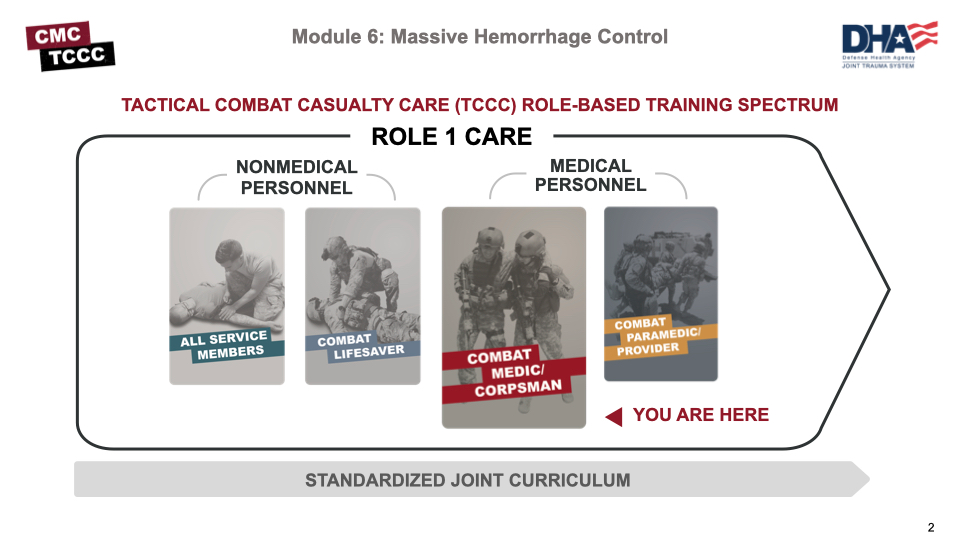
As a combat medic/corpsman, you are the first medical provider to care for the casualty and initiate more advanced treatments. As such, it is important that you understand the roles and responsibilities of the nonmedical personnel (ASM and CLS) that may be assessing casualties and providing care/assisting in care in the prehospital environment.
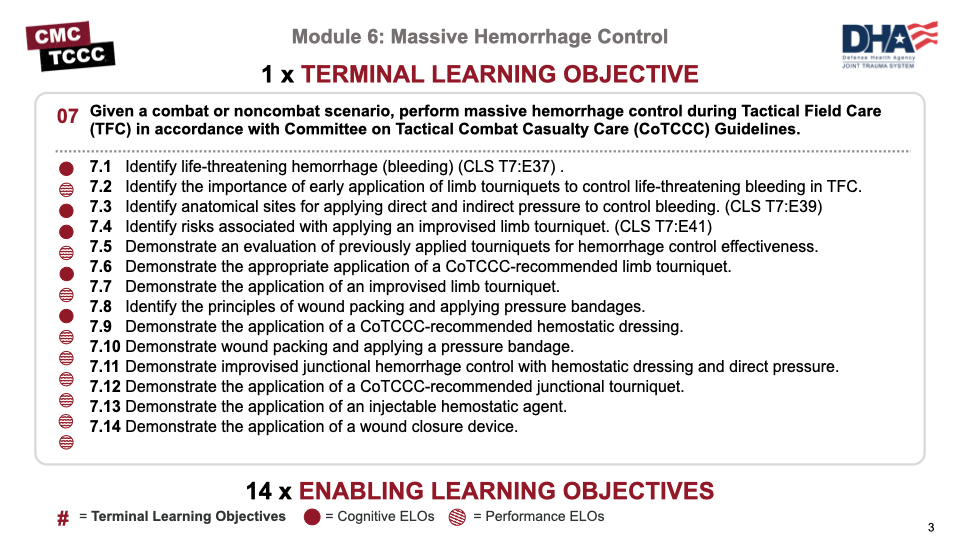
There are five cognitive and nine performance learning objectives for the Massive Hemorrhage Control module. The cognitive learning objectives are to identify:
- Life-threatening hemorrhage (bleeding)
- The importance of early application of limb tourniquets to control life-threatening bleeding
- Anatomical sites for applying direct and indirect pressure to control bleeding
- Risks associated with applying an improvised limb tourniquet
- The principles of wound packing
The performance learning objectives are to demonstrate:
- The evaluation of previously applied tourniquets for hemorrhage control effectiveness
- The appropriate application of a CoTCCC-recommended limb tourniquet
- The application of an improvised limb tourniquet
- The application of a CoTCCC-recommended hemostatic dressing
- Wound packing and application of a pressure bandage
- Improvised junctional hemorrhage control with a hemostatic dressing and direct pressure
- The application of a CoTCCC-recommended junctional tourniquet
- The application of an injectable hemostatic agent
- The application of a wound closure device
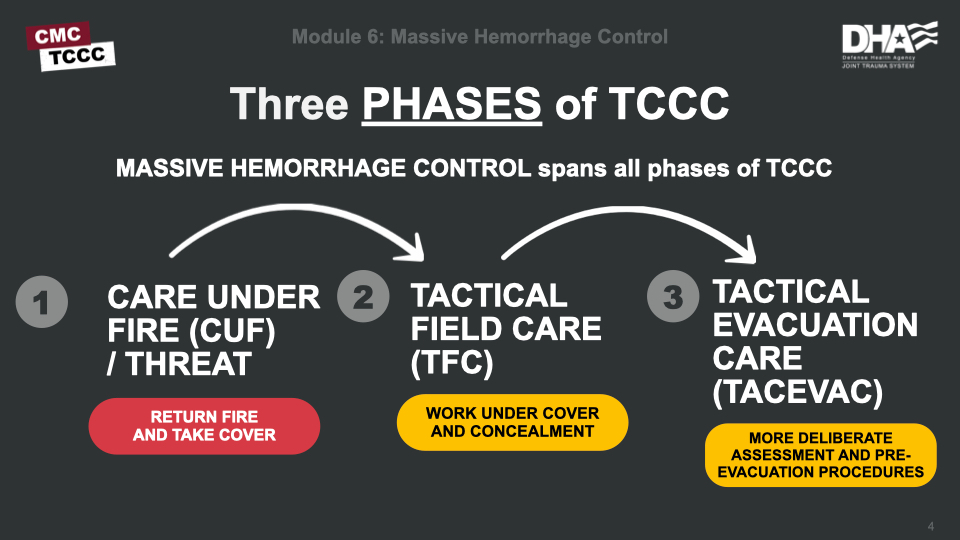
Massive hemorrhage should be identified and controlled as early as possible. It is typically addressed in Care Under Fire (CUF) with limb tourniquets and in Tactical Field Care (TFC) with the additional techniques that you will learn in this module.
That said, the casualty and any interventions should be continually reassessed throughout the phases of care and may require you to take action to ensure hemorrhage is controlled.
It is critical to be able to quickly identify life-threatening hemorrhage and promptly intervene in accordance with the CoTCCC guidelines.
In Care Under Fire, this typically means a quick survey for obvious life-threatening hemorrhage and the application of a high and tight (hasty) limb tourniquet.
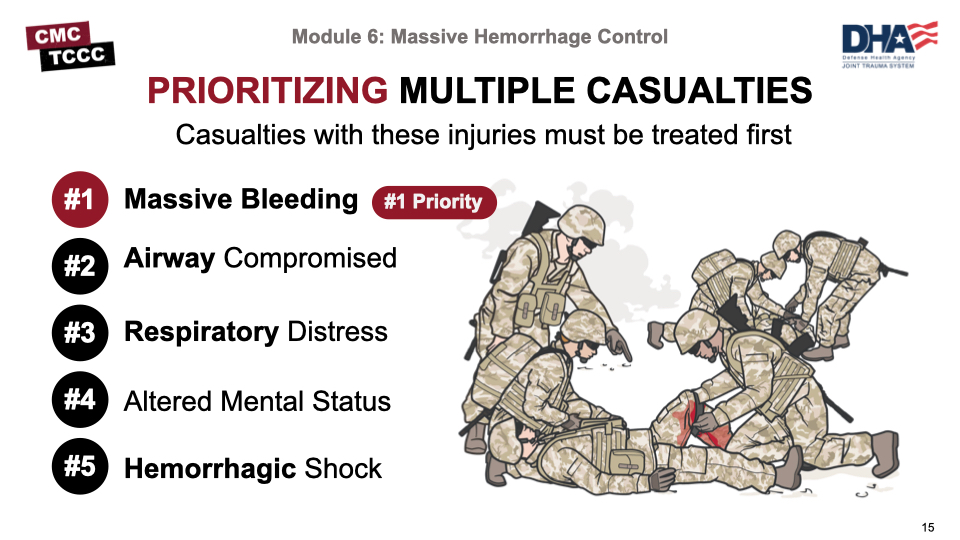
The relative safety and security and the additional time afforded in the Tactical Field Care phase allow for a more deliberate approach to assessment and treatment for the M in MARCH PAWS, which is Massive Bleeding and the #1 treatment priority.

This video provides an overview of the approach to assessment and treatment of massive hemorrhage in Tactical Field Care.
MASSIVE HEMORRHAGE OVERVIEW IN TFC
The combat medic/corpsman has more training and experience than nonmedic first responders (ASM and CLS) and an expanded scope of care in treating massive hemorrhage.
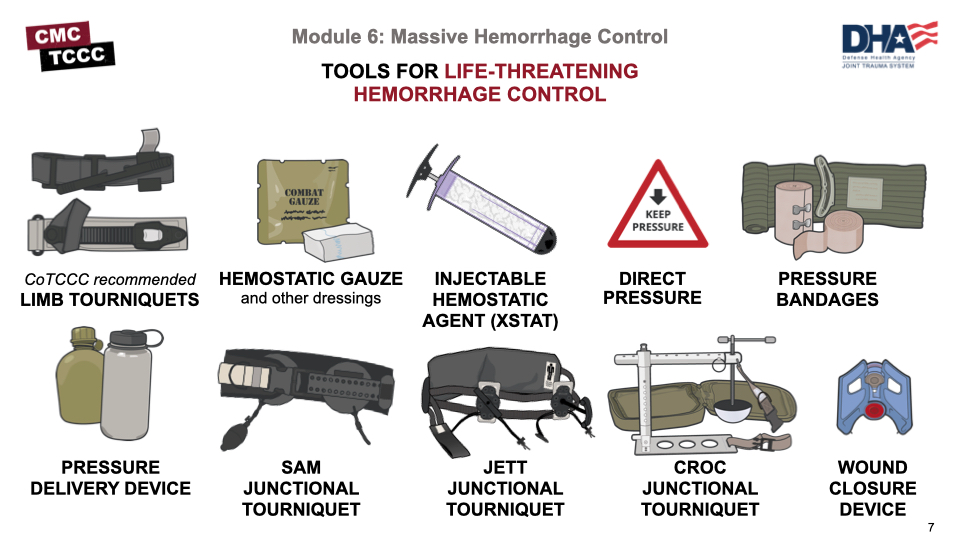
In addition to limb tourniquets, hemostatic dressings direct pressure, and pressure bandages, the CMC has additional tools including injectable hemostatic agents (XSTAT), junctional tourniquets, the IT Clamp, etc.
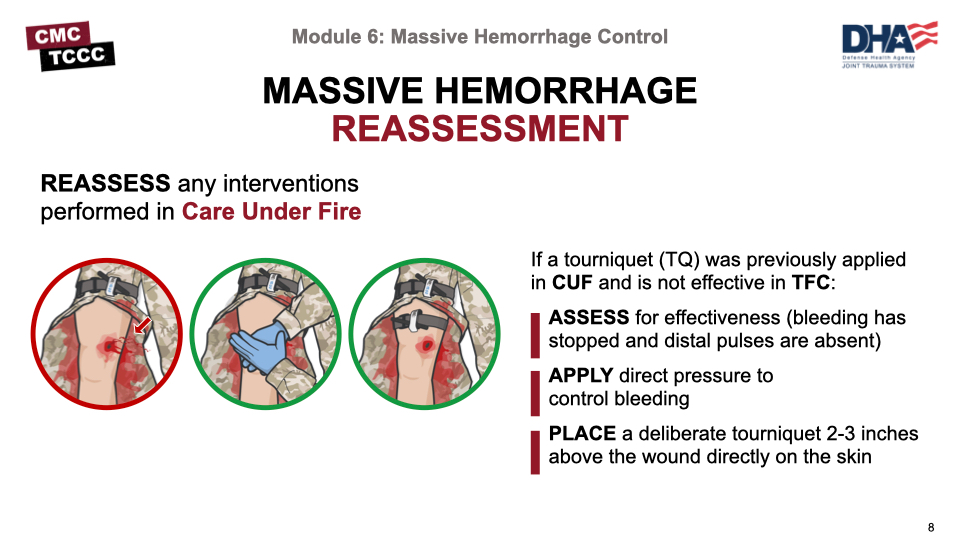
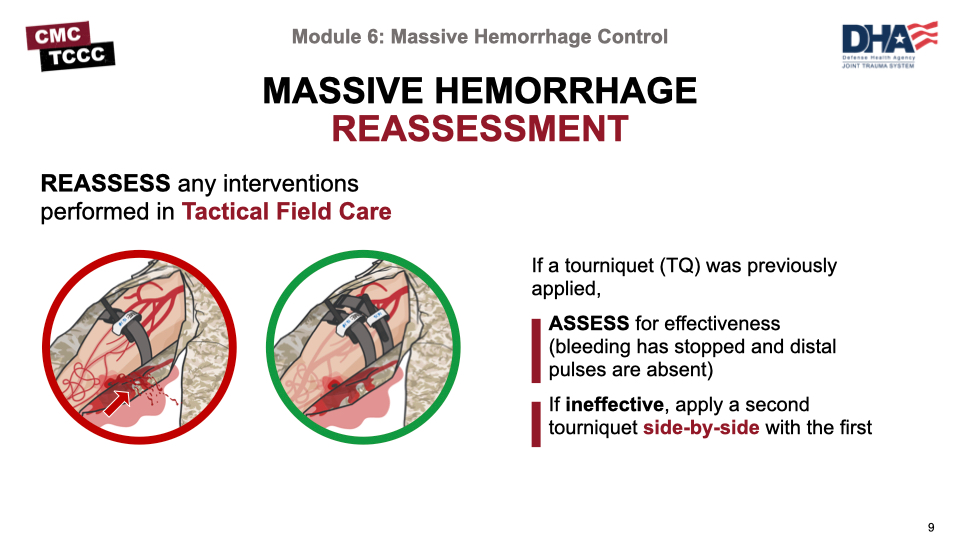
While completing the TTA, any interventions performed in Care Under Fire should be reassessed.
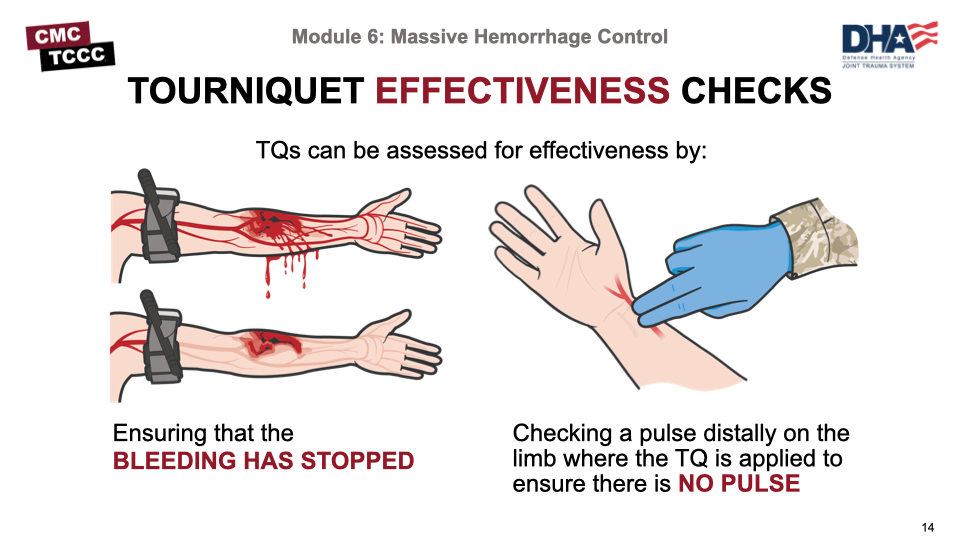
Previously applied tourniquets should be assessed for effectiveness (bleeding has been stopped and distal pulses are absent).
If the tourniquet is not effective, tighten the tourniquet and/or apply a second tourniquet side-by-side and proximal to the first one.
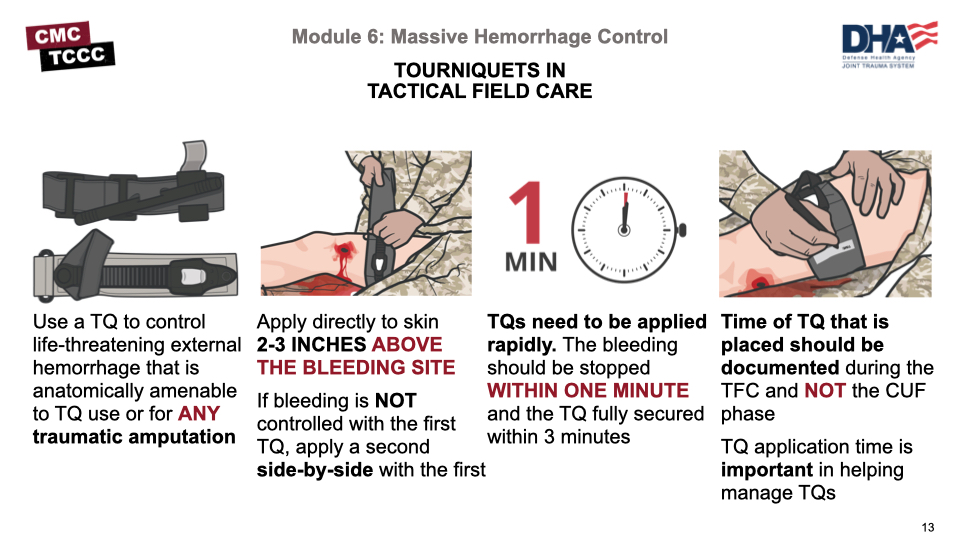
Assess for unrecognized hemorrhage and control all sources of bleeding. If not already done, use a CoTCCC-recommended limb tourniquet to control life-threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation. Apply directly to the skin 2-3 inches above the bleeding site. If bleeding is not controlled with the first tourniquet, apply a second tourniquet side-by-side with the first.
Body substance isolation (or BSI) is a situation-dependent consideration in TCCC.
For example, in Care Under Fire, there is no time to worry about body substance isolation, although your tactical gloves do offer some level of protection. However, once in Tactical Field Care, whenever possible, responders should don latex-free gloves as a BSI precaution.
Gloves are found in most equipment kits, including the JFAK, CLS bags, and combat medic aid bags.
Early identification of severe hemorrhage is critical. The below image shows signs of ongoing life-threatening bleeding that may not have been noted or appropriately addressed in Care Under Fire.
These include:
Pulsatile Bleeding
Also called Arterial bleeding is the most serious type of bleeding. Since arterial blood flows from the heart, it’s oxygenated and bright red. It will also shoot out with each heartbeat in a rhythmic pattern.
Steady Bleeding
In this type of bleeding, the blood flows steadily. If it's a large vein, the bleeding may be gushing. When a vein is cut, most veins will collapse, which helps to slow the bleeding. If it's a deep vein such as an iliac vein, the bleed can be just as difficult to control as an arterial bleed
Bright Red Blood Pooling on the Ground or Soaking Overlying Clothing
The color of blood you see can indicate where the bleeding might be coming from. In this case, bright red blood indicates that it is oxygenated and likely an arterial bleed.
Blood Flowing at the Site of a Traumatic Amputation of an Arm or Leg
There will be extensive bleeding due to all of the blood vessels involved may not be vasoconstrictive. A second type of traumatic amputation occurs when the limb becomes completely detached from the body. As much as 1 L of blood may be lost before the arteries spasm and become vasoconstrictive (less than 1 minute).
Ineffective Bandage
Bandages that become soaked with blood generally indicate that the injury requires a tourniquet or the bandage was not placed on the wound correctly.
Any obvious ongoing life-threatening bleeding should be addressed immediately.
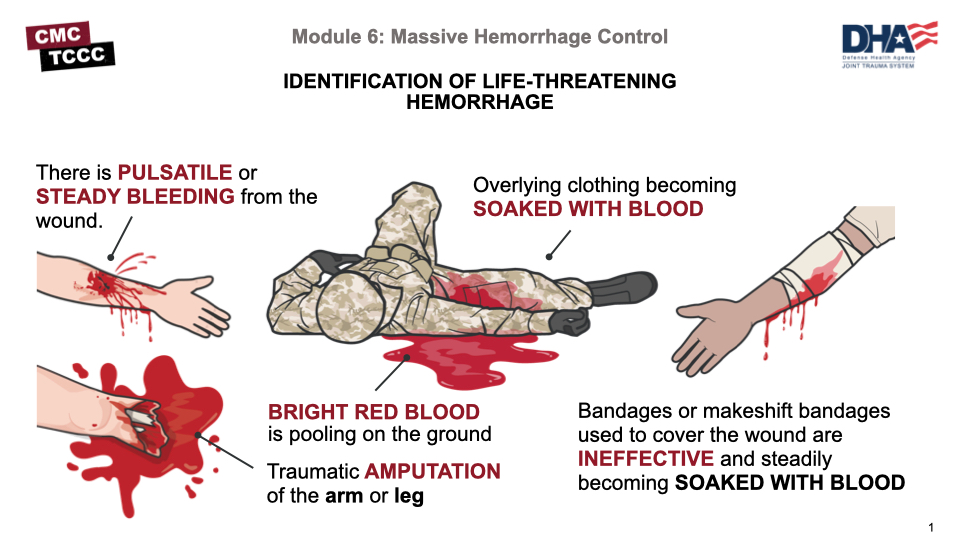
The below image talks about signs of ongoing life-threatening bleeding that may not have been noted or appropriately addressed in Care Under Fire. These include pulsatile blood, steady bleeding from the wound, blood pooling on the ground or soaking overlying clothing or bandages, or blood flowing at the site of a traumatic amputation of an arm or leg.
Any obvious ongoing life-threatening bleeding should be addressed immediately.
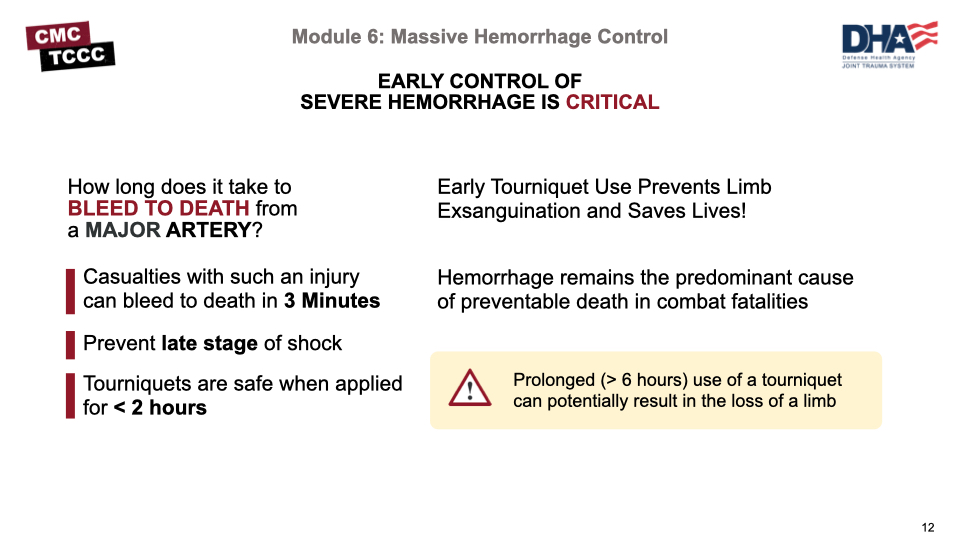
In combat casualties, early control of significant external hemorrhage is the most important intervention. Hemorrhage remains the predominant cause of preventable death in combat fatalities.
Early tourniquet use prevents limb exsanguination and saves lives. Nonindicated tourniquet placement is common (even when CUF is included as an indication), and morbidity is uncommon when tourniquet use is relatively brief.
- Expose the injury, assess the bleeding source (assess for unrecognized hemorrhage), and control all sources of bleeding.
- Control life-threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation.
- Remember: Bleeding should be stopped within 1 minute and the tourniquet fully secured within 3 minutes.
- The time of tourniquet placement should be documented on the tourniquet itself and on the DD 1380 in TFC (but not during CUF).
The effectiveness of a tourniquet can be assessed by ensuring that bleeding has stopped and by checking for a pulse distally on the limb from where the tourniquet has been applied.
If bleeding continues or you detect a pulse, tighten the existing tourniquet or apply a second tourniquet next to the first more proximally on the limb.
Because of their effectiveness at hemorrhage control, the speed with which they can be applied, and the lack of a requirement to hold sustained direct pressure on the bleeding site, tourniquets are the best option for temporary control of life-threatening extremity hemorrhage in the tactical environment
As mentioned in the prior modules, there may be more than one casualty and, as a combat medic, you may need to triage casualties and direct the actions of other responders before actually beginning individual casualty assessment. Triage ensures prioritization of available time, personnel, and medical supplies.
Massive bleeding is the #1 treatment priority.
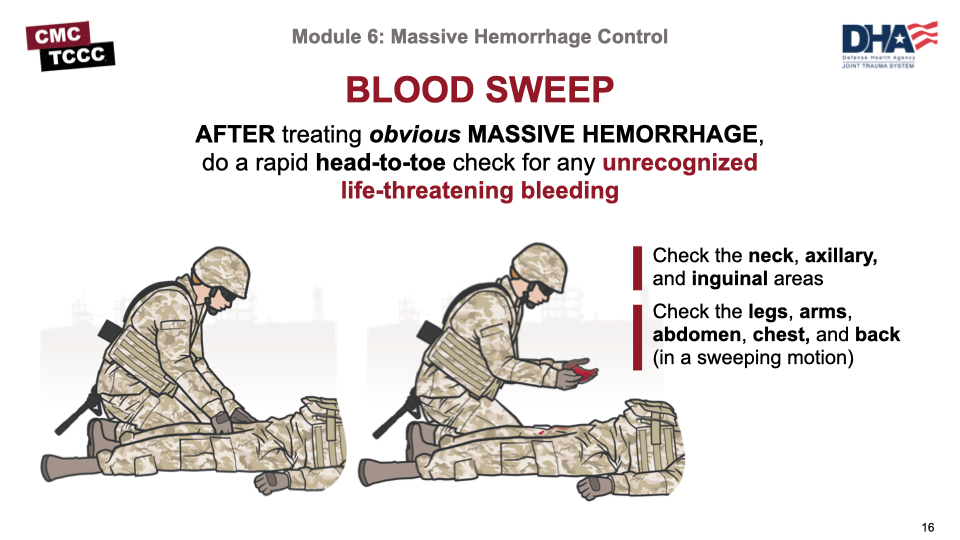
The Tactical Trauma Assessment (TTA), as you learned in the previous module, includes a head-to-toe check for any unrecognized life-threatening bleeding (called a blood sweep).
This blood sweep is a visual and hands-on inspection of the front and back of the casualty from head to toe, including the neck, armpits, and groin.
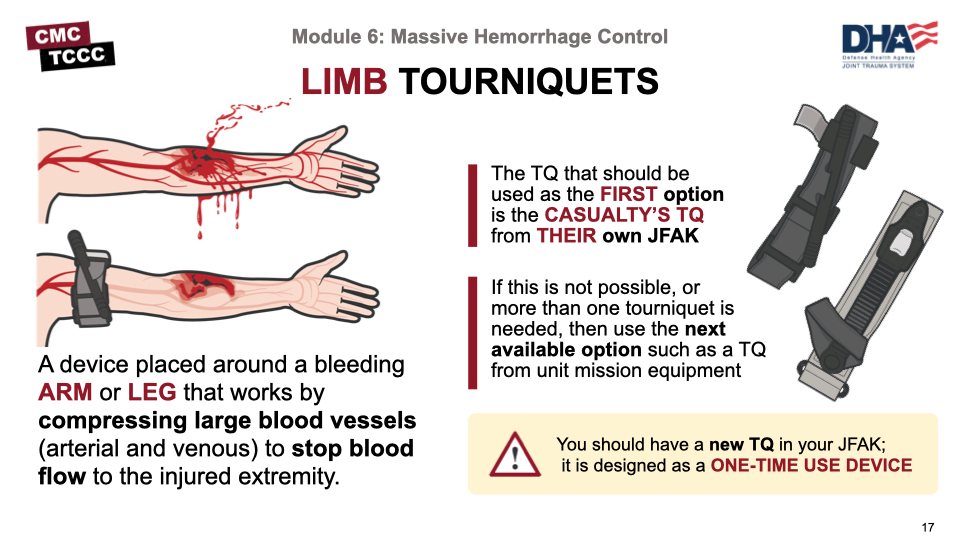
A tourniquet is a device that is placed around a bleeding arm or leg that works by compressing large blood vessels (arterial and venous) and stopping blood flow to the injured extremity.
A CoTCCC-recommended limb tourniquet (TQ) should be applied quickly to all wounds that are amenable when ongoing severe bleeding is noted. Use the casualty’s TQ from their JFAK first. If this is not possible, or more than one tourniquet is needed, then use the next available option such as a TQ from unit mission equipment. Remember that a tourniquet is designed as a one-time-use device.
Every Soldier should have a new TQ in their JFAK or medical kit. Never deploy with a tourniquet that has been used previously in training, as there is an increased risk of device failure.
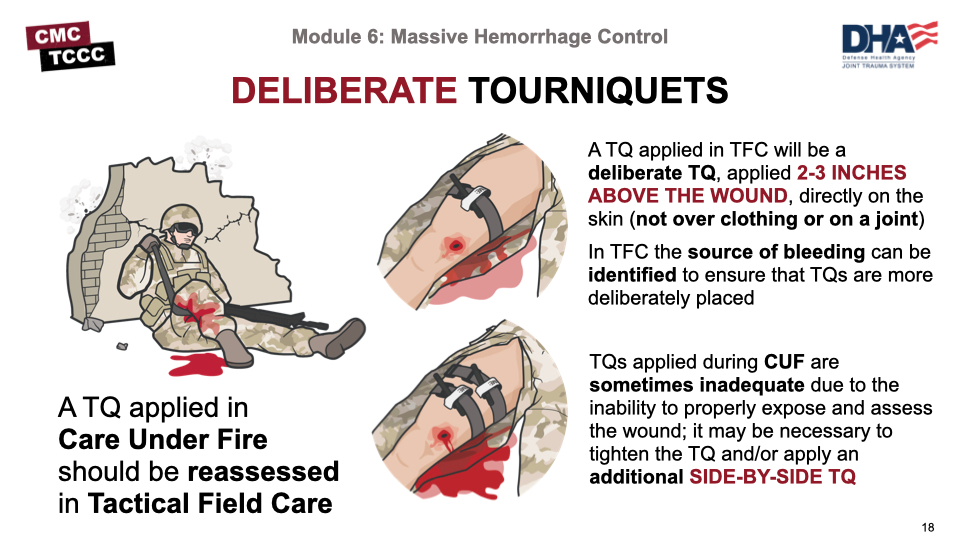
Tourniquets that were placed in CUF should be reassessed for effectiveness if the casualty reaches TFC. Also, tourniquets placed in CUF are often placed hastily, out of necessity, over clothing, and “high and tight” if the site of bleeding is not immediately obvious.
In TFC, there is more time to expose the wound and determine the actual site of bleeding. Tourniquets should be applied more deliberately in the TFC setting, 2 to 3 inches above the wound and directly on the skin to maximize effectiveness and minimize the amount of healthy tissue that might be impacted by a tourniquet placed too high on the limb.
If bleeding is not controlled and the distal pulse absent after the first tourniquet has been placed in either CUF or TFC, you may need to tighten the tourniquet and/or apply a second tourniquet side-by-side and proximal on the limb to the first.
Remember: Do not put tourniquets over the knee, elbow, a holster or other equipment, or a cargo pocket containing bulky items.
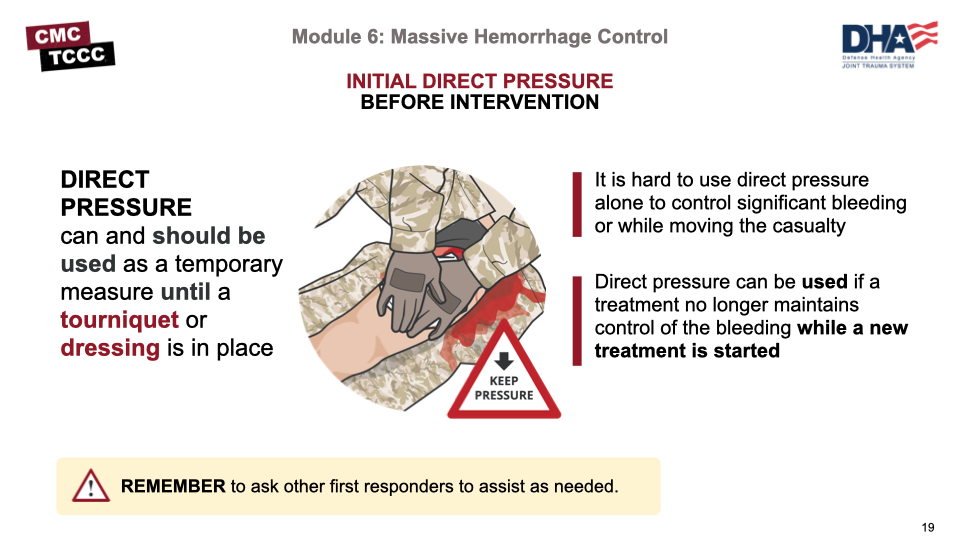
Direct pressure can effectively control bleeding and should be used as a temporary measure until a tourniquet or dressing can be applied.
It is hard to use direct pressure alone to control significant bleeding or while moving a casualty but it should be attempted while gathering and preparing equipment for more definitive treatments.
Do not forget to ask other first responders to assist as needed.
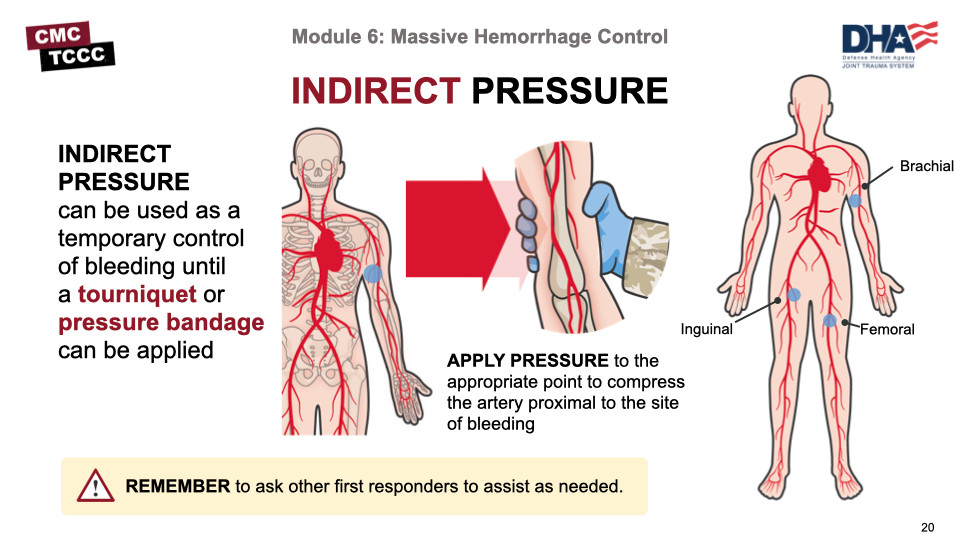
Indirect pressure can also be used as a temporary measure to effectively control bleeding until a tourniquet or pressure bandage can be applied. It involves applying pressure to the appropriate pressure point to compress the artery proximal to the site of bleeding.
As with direct pressure, it is hard to use indirect pressure alone to control significant bleeding or while moving a casualty but it should be attempted while gathering and preparing equipment for more definitive treatments.
Do not forget to ask other first responders to assist as needed.
This video demonstrates the two-handed application of a ratchet tourniquet in TFC.
TWO-HANDED RATCHET TOURNIQUET IN TFC
This video demonstrates the two-handed application of a windlass tourniquet in TFC.
TWO-HANDED WINDLASS TOURNIQUET IN TFC
In this skill station we will demonstrate and practice hemorrhage control techniques including the application of CoTCCC-recommended windlass and ratchet limb tourniquets as well as improvised limb tourniquets.
Remember: CoTCCC-recommended limb tourniquets should be used whenever possible.
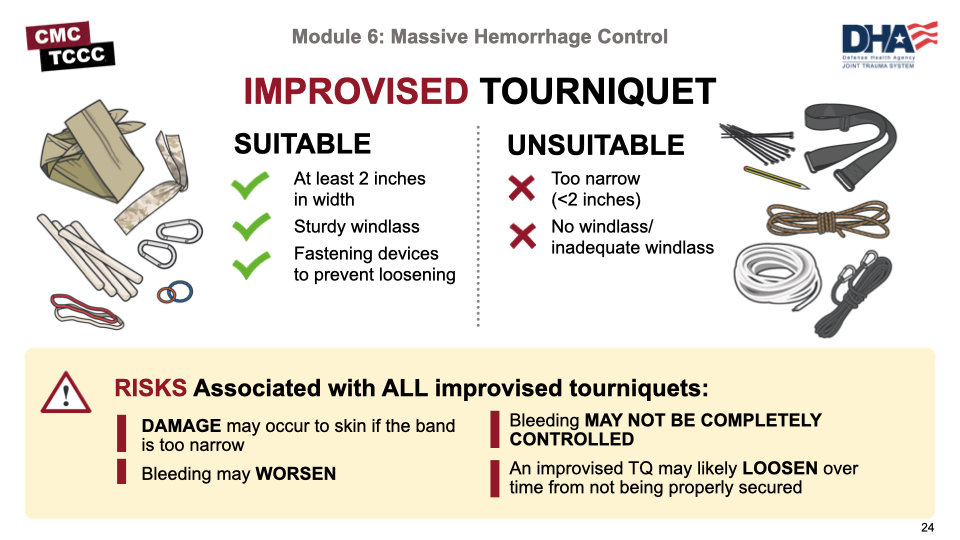
Improvised tourniquets should only be used as a last resort when there is no other available option to control life-threatening extremity hemorrhage. Improvised tourniquets may not be effective in controlling bleeding, may loosen after placement, and could cause tissue damage if too narrow.
An improvised tourniquet is an absolute last resort!
If an improvised tourniquet must be used, use materials at least 2 inches in width to avoid tissue damage, continue to reassess after placement as they are prone to loosening, and apply a CoTCCC-recommended tourniquet as soon as one becomes available.
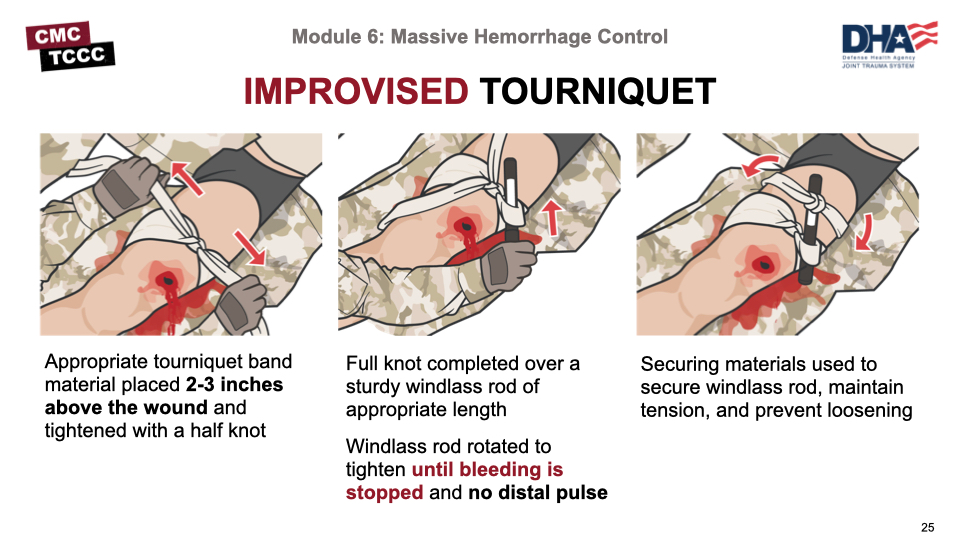
The below image shows the proper application of an improvised tourniquet used as a last resort to control life-threatening hemorrhage.
Note that the tourniquet band material used is at least 2 inches in width, that a sturdy windlass rod of appropriate length is used to ensure adequate tension can be applied and maintained, and that a securing device is used to secure the windlass in place and maintain tension.
This video demonstrates the application of an improvised limb tourniquet.
IMPROVISED LIMB TOURNIQUET
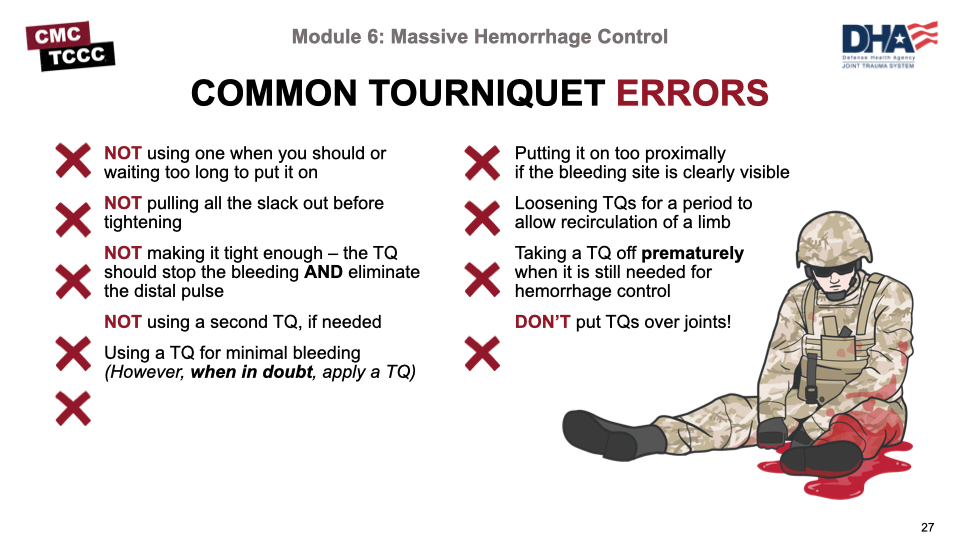
Several common errors should be avoided in using tourniquets. These include:
- Not using or waiting too long to use a tourniquet when indicated
- Not removing all of the slack before tightening the tourniquet
- Not tightening the tourniquet enough to stop bleeding and eliminate the pulse
- Not using a second tourniquet if needed
- Using a tourniquet when one is not needed
- Putting a tourniquet “high and tight” rather than 2-3 inches above the wound when the bleeding site is clearly visible
- Loosening tourniquets for a period of time to allow recirculation of blood to an injured limb
- Removing a tourniquet prematurely when it is still needed for hemorrhage control
- Placing tourniquets over knee or elbow joints.
Remember: Tourniquets hurt when applied properly.
For external hemorrhage from sites not amenable to limb tourniquets (places where a tourniquet cannot be effectively applied) or for bleeding from wounds not requiring a tourniquet, use a CoTCCC-recommended hemostatic gauze. Hemostatic gauze with or without a pressure bandage can even be used to control compressible junctional hemorrhage (such as the neck, axillary, inguinal areas), which will be discussed later in this module.
Hemostatic gauze should not be packed into chest wounds.
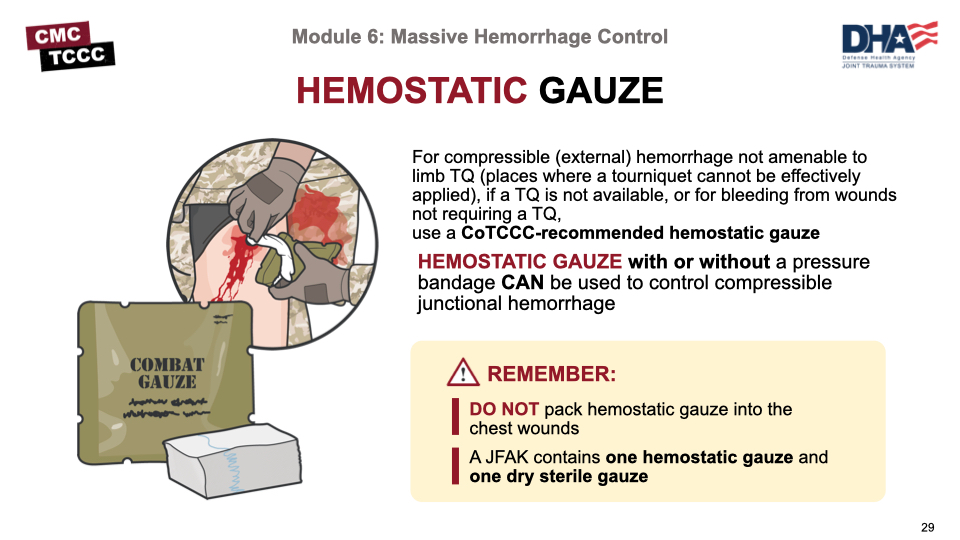
CoTCCC-recommended hemostatic gauze dressings, including Combat Gauze, ChitoGauze, and Celox Gauze, are safe and contain active ingredients that assist with blood-clotting at the site of active bleeding.
To effectively form a clot and stop bleeding, hemostatic gauze must be packed into the wound to maximize contact at the active source of bleeding with direct pressure applied over the wound for at least 3 minutes.
Note: Although both ChitoGauze and Celox contain Chitosin, which is a shellfish derivative, they will not cause an allergic reaction in casualties with a shellfish allergy.
Even with the active hemostatic agents in hemostatic dressings, wound packing and direct pressure are required to control bleeding.
Whenever possible, identify the exact source of bleeding and apply direct pressure as a temporary measure while preparing hemostatic gauze for placement. Pack the wound maximizing contact between the hemostatic gauze and the active site of bleeding. Maintain constant direct pressure at the source of bleeding while packing the wound. After the wound has been packed, hold direct pressure over the gauze on the wound for at least 3 minutes. This is necessary even with the active hemostatic agent in the gauze.
When packing a large wound, more than one hemostatic gauze and/or additional gauze may be needed. Carefully observe the wound to determine if bleeding has been effectively controlled. Once bleeding has been controlled, apply a pressure bandage.
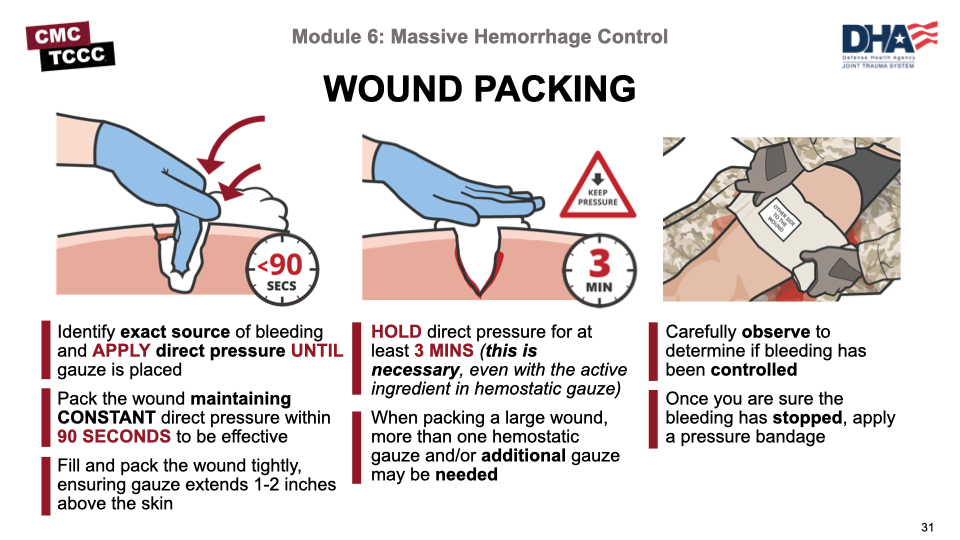
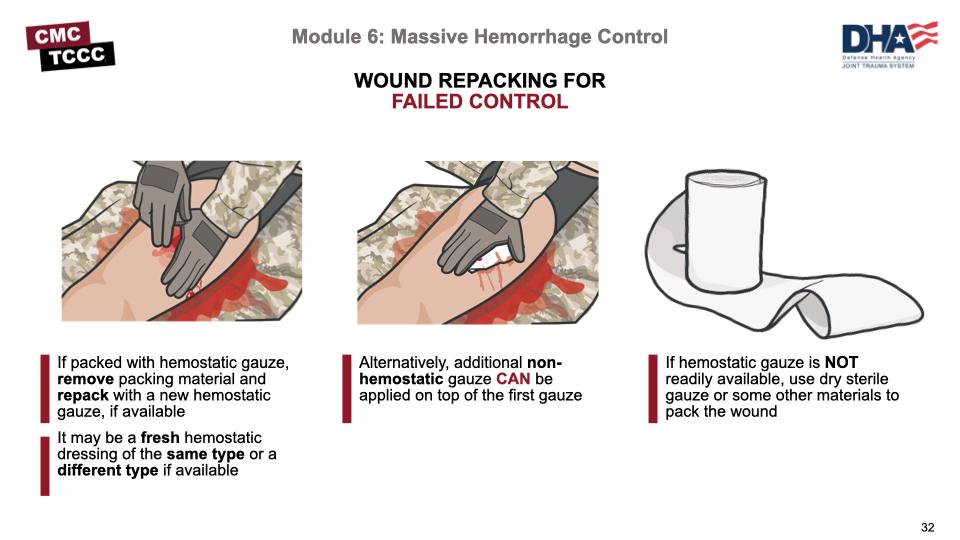
If a wound packed with hemostatic gauze continues to bleed after 3 minutes of direct pressure, remove the packing material and repack with a new hemostatic dressing if available.
If additional hemostatic gauze is not available or the wound was packed with a non-hemostatic gauze dressing, reinforce the dressing with additional non-hemostatic gauze and apply direct pressure and a pressure bandage until bleeding is controlled.
This video demonstrates the technique for application of wound packing with a hemostatic dressing.
HEMOSTATIC DRESSING AND WOUND PACKING
All dressings for significant bleeding should be secured with a pressure bandage. Maintain pressure on the wound throughout the process of applying the pressure bandage.
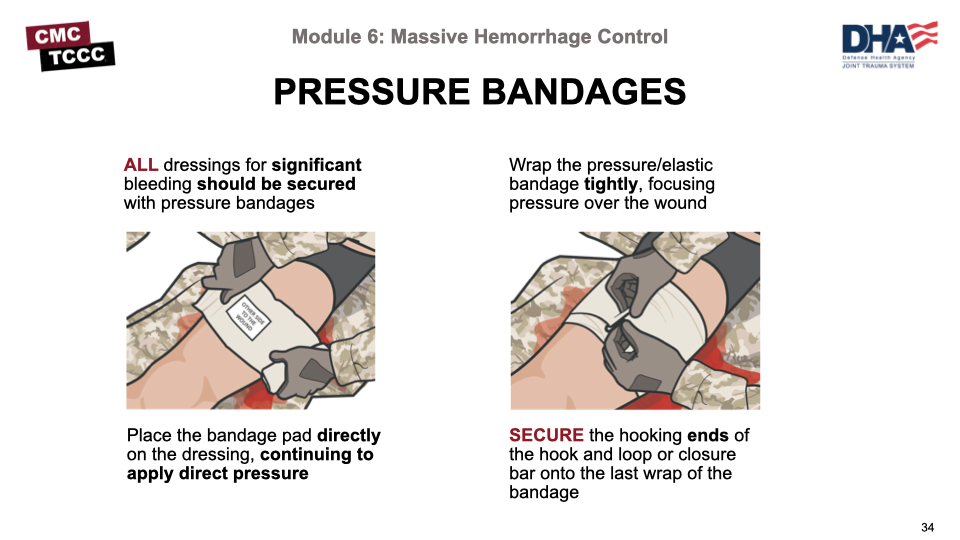
Remember: a pressure bandage should be tight but is not supposed to be a tourniquet.
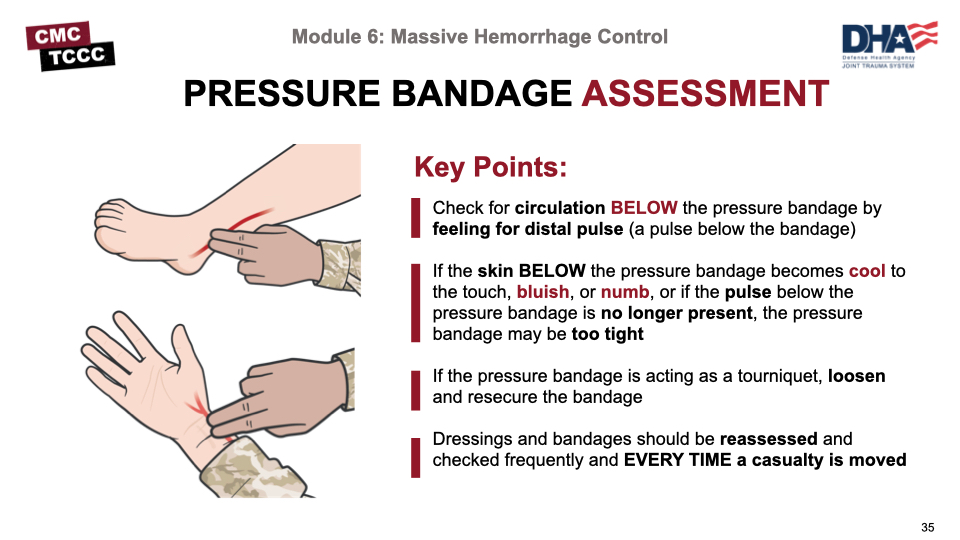
After applying a pressure bandage, check for circulation distal to the bandage. If the skin below the bandage is cool, bluish in color, or numb indicating decreased circulation or if the distal pulse is absent, the pressure bandage may be too tight. The pressure bandage should be loosened and resecured.
All dressing and bandages should be reassessed frequently and especially after a casualty has been moved.
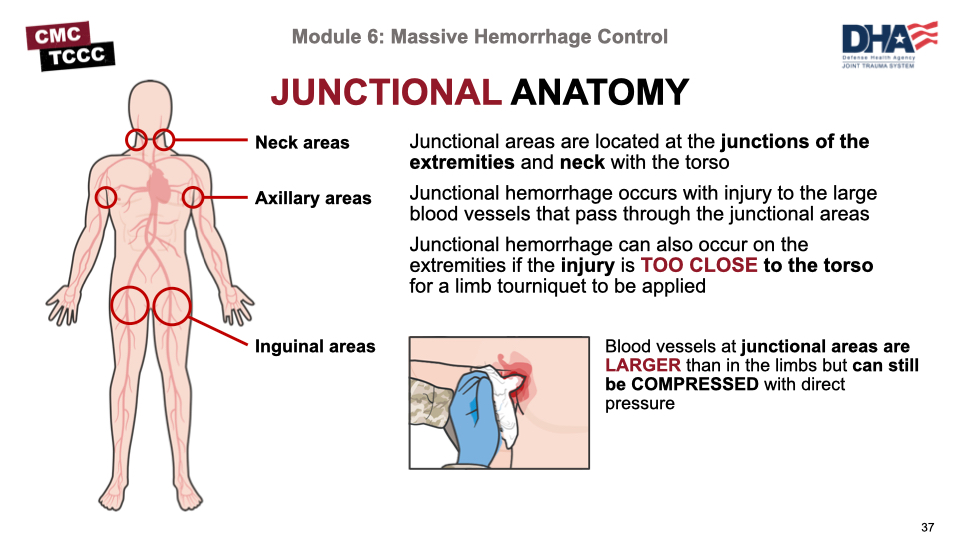
Junctional areas are located at the junctions of the extremities and neck with the torso. Junctional hemorrhage occurs with injury to the large blood vessels that pass through the junctional areas or on the extremities themselves if the injury is too close to the torso to allow for a limb tourniquet to be applied.
Junctional hemorrhage is compressible external hemorrhage and must be treated without delay. Although blood vessels at the junctional areas are larger than in the limbs, they can still be compressed, and a hemostatic dressing and direct pressure should be applied immediately.
The areas where the neck and the limbs join the torso are “junctional” areas. Hemorrhage from wounds in these areas cannot be controlled by application of limb tourniquets like the C.A.T.
Junctional tourniquets are designed to stop bleeding at the junctional areas. If the bleeding site is amenable, a junctional tourniquet should be applied immediately.
Do not delay in applying a junctional tourniquet once it is ready for use. The wound should be packed with a hemostatic dressing with direct pressure while the tourniquet is readied for use.
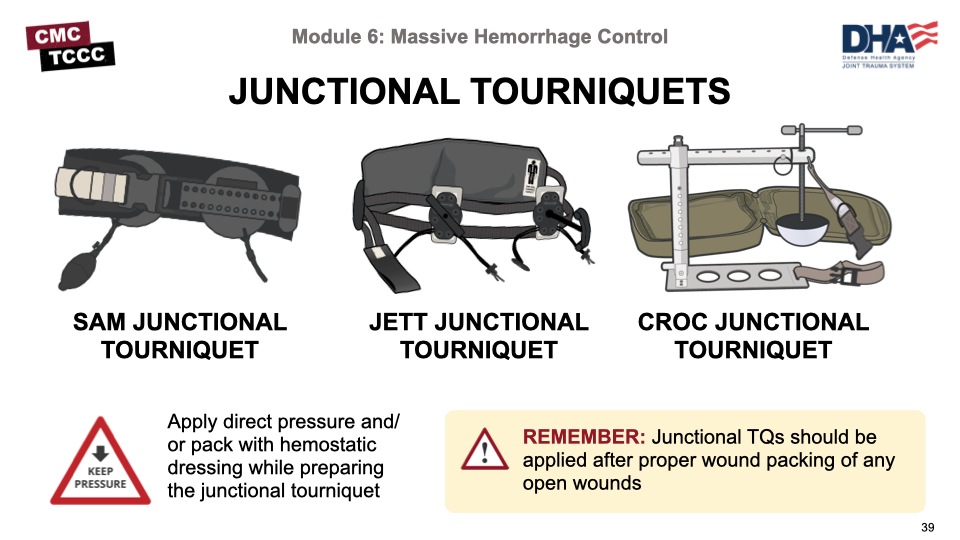
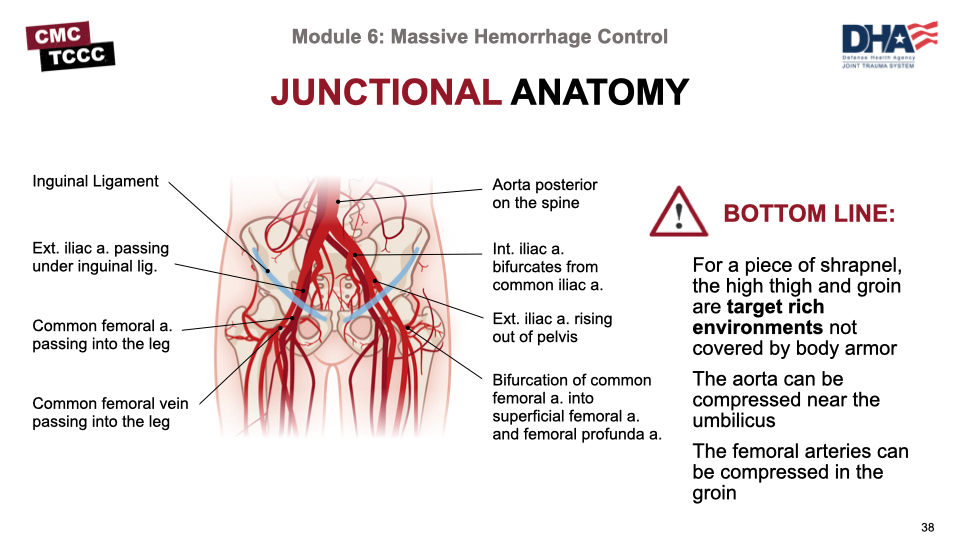
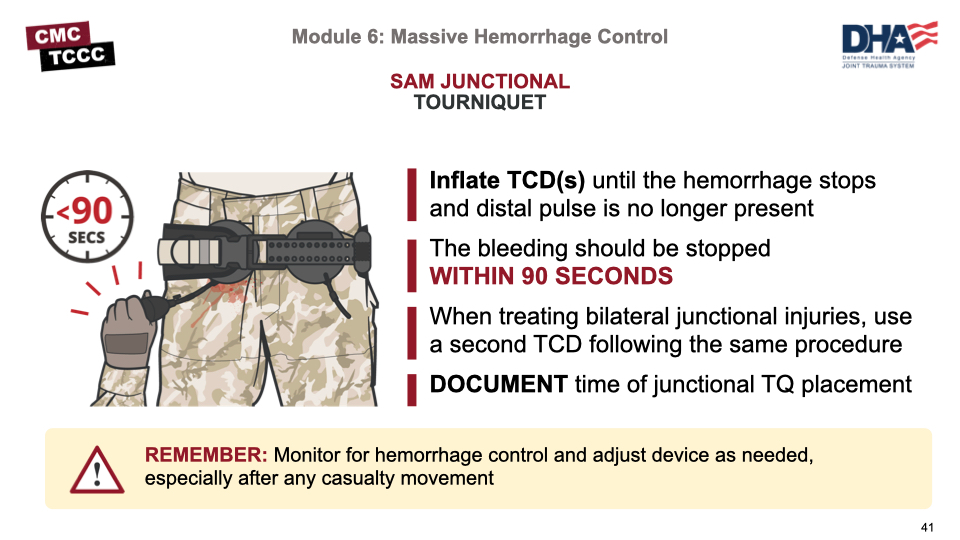
The SAM Junctional Tourniquet is one of the three CoTCCC-recommended junctional tourniquets. It is designed to provide pelvic compression (with the circumferential belt) as well as direct pressure over inguinal junctional wounds with the targeted compression devices (TCDs).
It is important for the combat medic/corpsman to have an understanding of basic junctional anatomy to ensure the TCDs are positioned appropriately to compress the large blood vessels and effectively control bleeding.
For inguinal junctional hemorrhage, the TCDs should be positioned over the femoral pulse just below the inguinal ligament or just below the midpoint of the imaginary line between the anterior superior iliac spine and pubic tubercle, if femoral pulse is not palpable.
Once the TCDs are appropriately positioned, the belt is buckled and all slack is removed from the belt before TCD inflation.
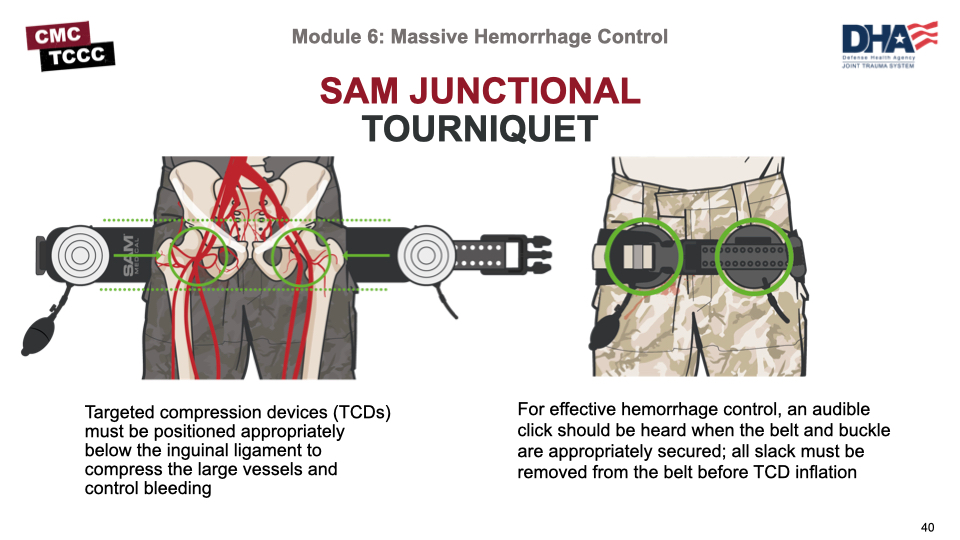
Once positioned and secured, a hand pump is used to inflate the TCD(s) until the hemorrhage stops and a distal pulse is no longer present.
Bleeding should be stopped within 90 seconds.
When treating bilateral junctional injuries, a second TCD can be used following the same procedure.
This video demonstrates the technique for use of the SAM Junctional Tourniquet to control massive hemorrhage from a junctional wound.
SAM JUNCTIONAL TOURNIQUET
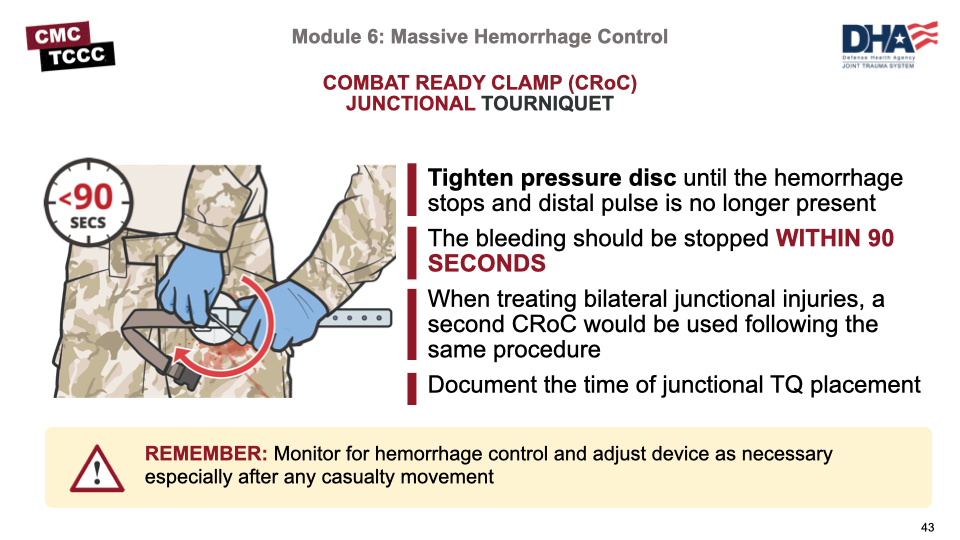
The Combat Ready Clamp is the third CoTCCC-recommended junctional tourniquet. It is designed to provide direct pressure over junctional wounds with the pressure disc.
The pressure disc should be positioned over the femoral pulse just below the inguinal ligament or just below the midpoint of the imaginary line between the anterior superior iliac spine and pubic tubercle, if femoral pulse is not palpable.
If the wound was not previously packed, a gauze dressing should be placed over the desired pressure point.
The pressure disc is tightened on the injured side until bleeding has stopped and distal pulse is no longer palpable. Monitor for hemorrhage control and adjust the device as needed especially after any casualty movement.
To treat bilateral junctional injuries, a second CRoC device would be used following the same procedure.
This video demonstrates the application of a CoTCCC-recommended junctional tourniquet.
COMBAT READY CLAMP (CRoC) JUNCTIONAL TOURNIQUET
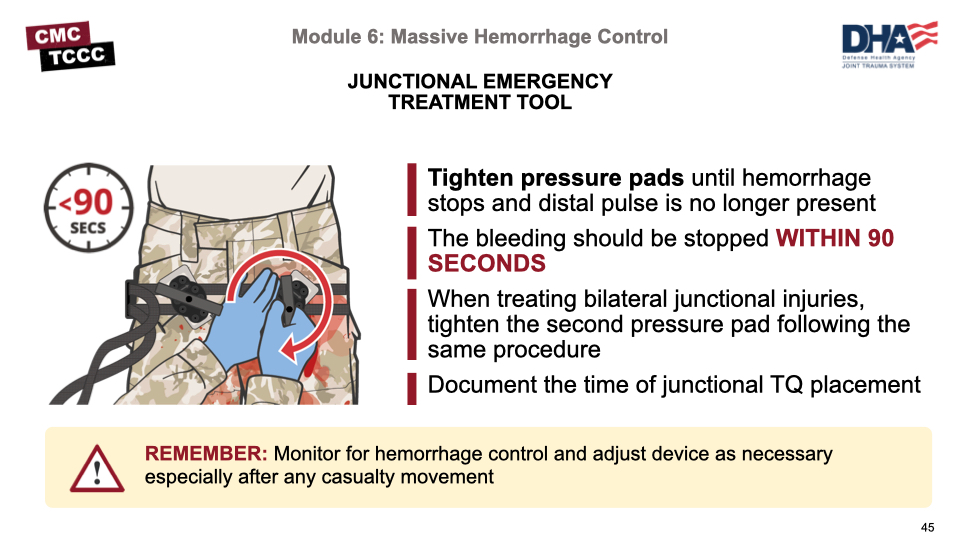
The Junctional Emergency Treatment Tool (JETT) is another of the three CoTCCC-recommended junctional tourniquets. Similar to the SAM, it is designed to provide pelvic compression (with the circumferential belt) as well as direct pressure over inguinal junctional wounds with the junctional pressure pads.
The junctional pressure pads should be positioned over the femoral pulse just below the inguinal ligament or just below the midpoint of the imaginary line between the anterior superior iliac spine and pubic tubercle, if femoral pulse is not palpable.
Adjust the two junctional pressure pads on the straps to position them in the area over the femoral pulse just below the inguinal ligament. Angle the junctional pressure pads so that their long axis is lined up with (parallel to) the inguinal canal or gutter (the distal part of the pad will be pointed somewhat laterally at approximately a 30-degree angle).
Once the pads are appropriately positioned, the belt is buckled and all slack should be removed from the belt before tightening the threaded T handle on the injured side until bleeding has stopped and distal pulse is no longer palpable.
This video demonstrates the application of a CoTCCC-recommended junctional tourniquet.
JUNCTIONAL EMERGENCY TREATMENT TOOL (JETT)
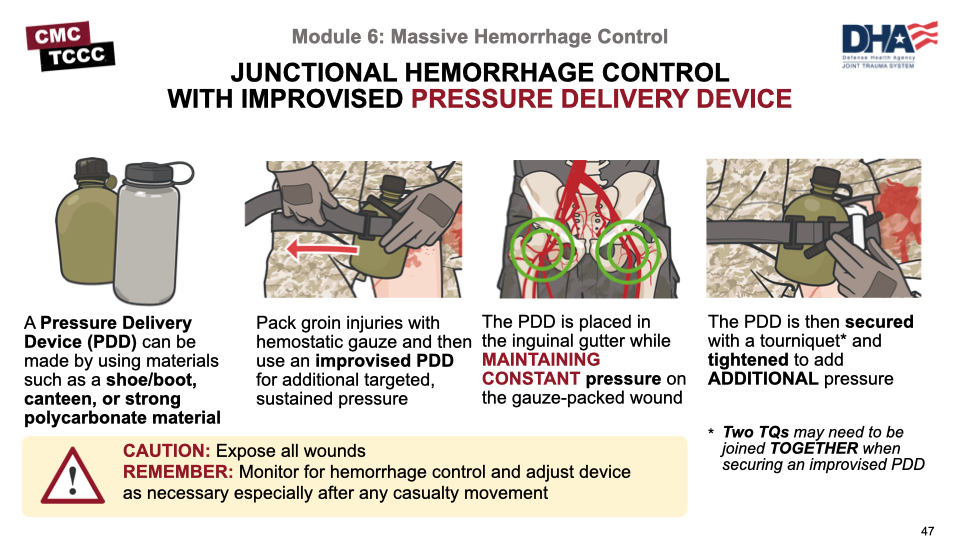
A casualty can die from massive hemorrhage quickly due to bleeding from junctional hemorrhage. If a junctional tourniquet is not available, apply a hemostatic dressing and direct pressure immediately.
An improvised junctional pressure delivery device (PDD) may be needed to apply additional, targeted, and sustained pressure to control junctional bleeding. An improvised PDD can be made using materials that are readily available on the battlefield, including limb tourniquets, water bottles, canteens, boots, shoes, etc.
The PDD is placed in the inguinal gutter while continuously maintaining pressure on the gauze-packed wound. The PDD is then secured using two limb tourniquets joined together around the casualty’s body and around the PDD. When the TQ windlass is tightened, additional pressure is applied to the PDD over the wound until the bleeding is stopped and the distal pulse is absent.
This video demonstrates the technique for use of an improvised junctional PDD to control massive hemorrhage from a junctional wound.
INGUINAL IMPROVISED JUNCTIONAL PDD
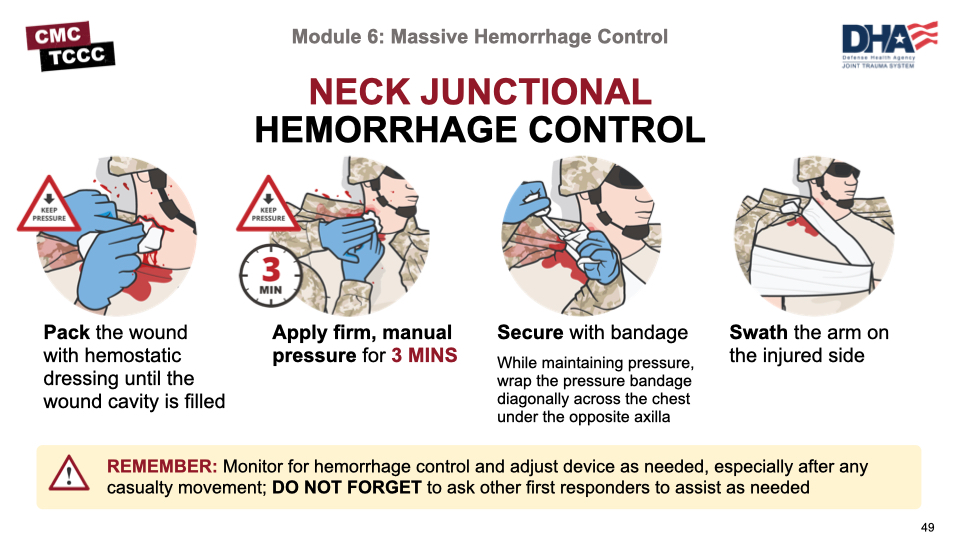
Junctional hemorrhage from a wound to the neck can be challenging to treat in TFC. The wound should be exposed, packed with hemostatic gauze until the wound cavity is filled1-2 inches above the skin, and firm, manual pressure should be applied continuously for a minimum of 3 minutes.
After bleeding has been controlled, continue to maintain pressure on the wound. Apply a pressure bandage by wrapping an elastic bandage over the wound on the neck on the affected side, diagonally across the body and under the opposite armpit, and then secure it with a nonslip knot. Swath the upper arm on the injured side to the chest using a cravat or another bandage.
Continue to reassess for hemorrhage control especially after casualty movement. Do not forget to ask other first responders to assist as needed.
This video demonstrates the technique for neck junctional hemorrhage control.
NECK JUNCTIONAL HEMORRHAGE CONTROL
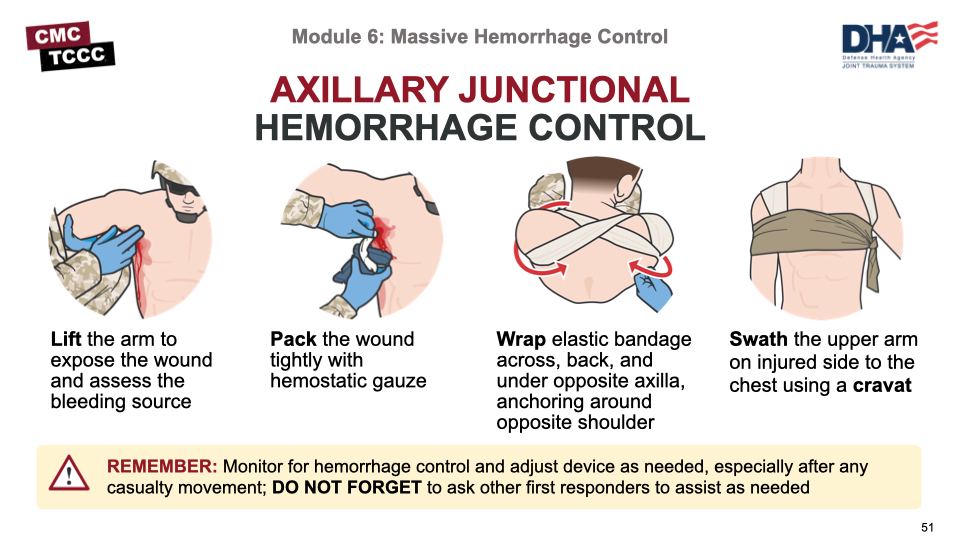
As with neck wounds, junctional hemorrhage from a wound to the axilla can be similarly challenging to treat in TFC.
The wound should be exposed, packed with hemostatic gauze mounded to at least 1-2 inches above the skin, and direct pressure applied continuously for a minimum of 3 minutes.
After bleeding has been controlled, continue to maintain pressure on the wound. Wrap a pressure (or elastic) bandage circumferentially around the shoulder and under the armpit twice on the affected side, ensuring that the hemostatic dressing underneath is completely covered. Wrap the pressure (or elastic) bandage diagonally across the body and under the opposite armpit and around the shoulder, and back across the body in a “figure 8” technique. Secure it with a nonslip knot or a securing device (depending on what type of bandage is used). Swath the upper arm on the injured side to the chest using a cravat.
The “figure 8” elastic bandage helps to maintain pressure on the wound when both arms are down at the casualty’s side. Continue to reassess for hemorrhage control, especially after casualty movement.
Do not forget to ask other first responders to assist as needed.
This video demonstrates the technique for axillary junctional hemorrhage control.
AXILLARY JUNCTIONAL HEMORRHAGE CONTROL
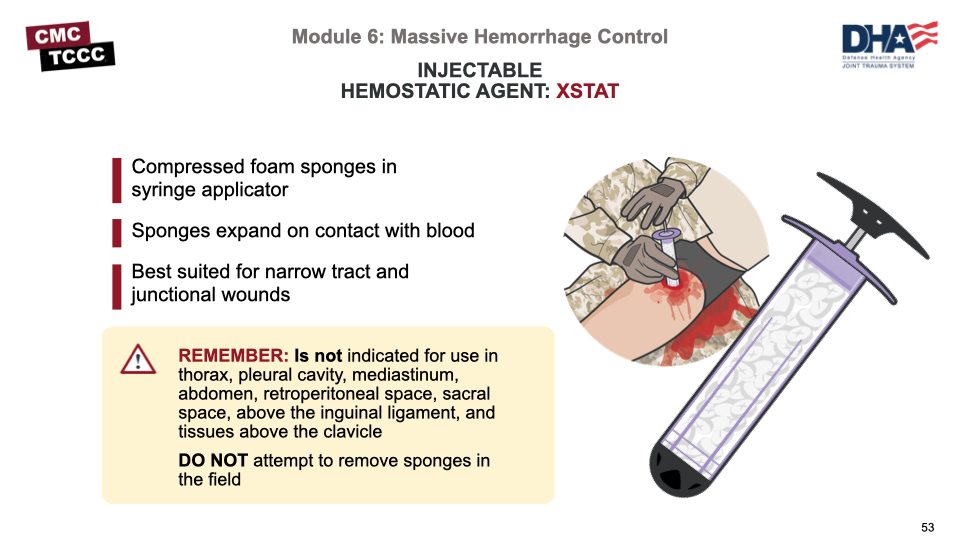
The injectable hemostatic agent XStat consists of an applicator syringe filled with small compressed foam sponges that expand when they come into contact with blood.
It offers another option for controlling external hemorrhage and is best suited for deep narrow tract and junctional wounds that are otherwise difficult to compress with external pressure.
This device is not indicated for use in the thorax, pleural cavity, mediastinum, abdomen, retroperitoneal space, sacral space, above the inguinal ligament, and tissues above the clavicle.
Do not attempt to remove sponges in the field.
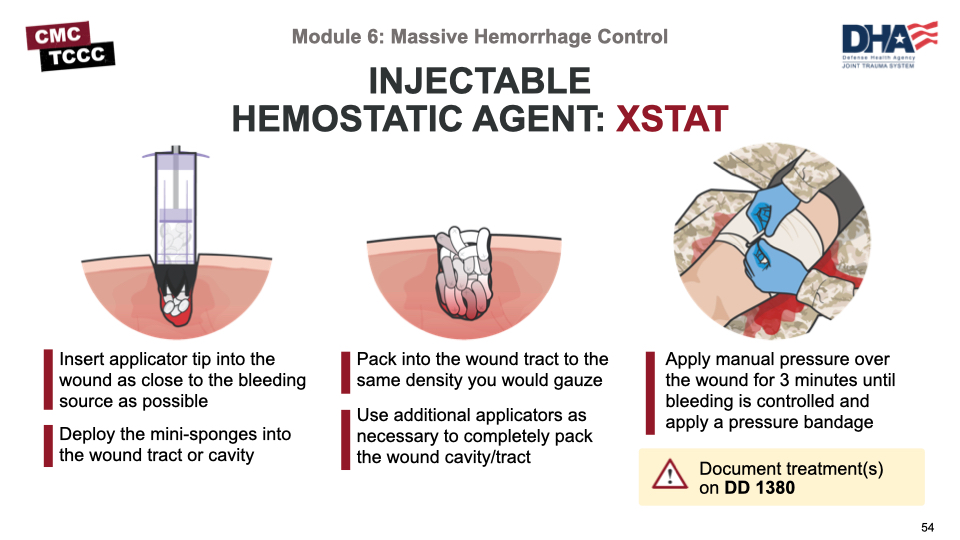
Although the expansion of the sponges within the wound cavity is designed to create internal pressure at the bleeding site, direct pressure should be applied to the wound for 3 minutes after application and a pressure bandage would be placed over the wound.
As with all treatments, it is important to document use of injectable hemostatic agent as the sponges are only for temporary use and will need to be removed surgically at a higher level of care.
This video demonstrates the technique for application of injectable hemostatic agent to control hemorrhage.
INJECTABLE HEMOSTATIC AGENT (XSTAT)
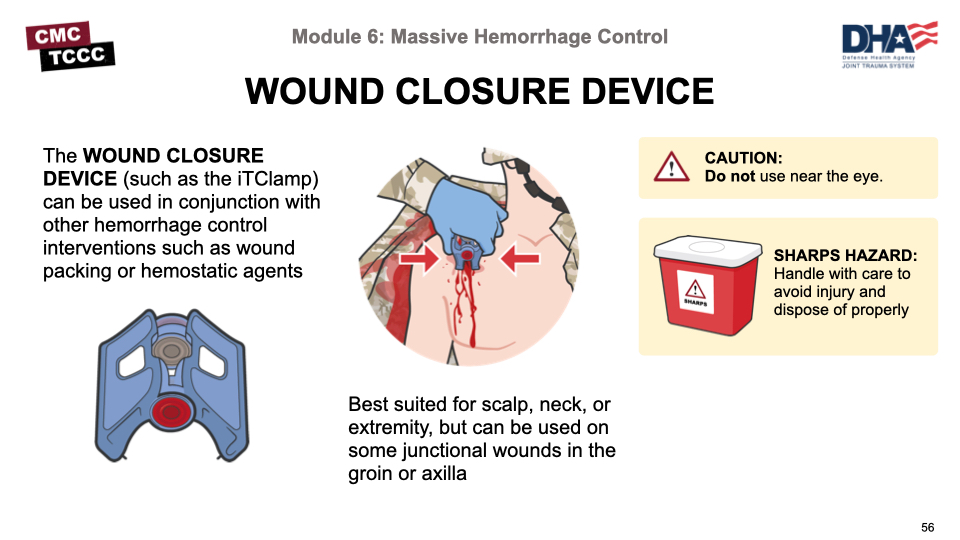
The wound closure device offers another option for controlling external hemorrhage. It is a clamping device that temporarily closes the wound edges to enable stable clot formation and mitigate further blood loss. It can be used with or without wound packing and hemostatic gauze for temporary wound closure and bleeding control.
It is best suited for wounds on the scalp, neck, or extremities but can also be used on some junctional wounds in the groin or axilla. The device can be applied quickly and can be removed and reapplied easily as needed in the prehospital environment.
For larger wounds or wounds with a cavity, more than one closure device and/or wound packing with hemostatic gauze before closure may be needed to control bleeding.
Identifying and controlling massive hemorrhage (the M in MARCH PAWS) remains the priority in Tactical Field Care.
All limb tourniquets hastily placed high and tight in CUF need to be reassessed and deliberate tourniquets placed for any extremity hemorrhage not previously addressed.
Junctional hemorrhage is compressible external hemorrhage not amenable to limb tourniquets and must be treated without delay using CoTCCC-recommended junctional tourniquets or improvised junctional hemorrhage control techniques with hemostatic dressings and direct pressure.
Other methods for addressing massive hemorrhage include injectable hemostatic agents and wound closure devices.
To close out this module, check your learning with the questions below (answers under the image).
Answers
What is the proper distance a deliberate tourniquet should be placed from the bleeding site in TFC?
A deliberate tourniquet placed in TFC should be 2-3 inches above (proximal) to the site of bleeding.
What are the differences between the high & tight/hasty tourniquets placed in CUF and the deliberate tourniquets placed in TFC?
The tourniquets placed in CUF are typically placed over the uniform/clothing as high up on the extremity as possible, as time is very limited and the exact site of bleeding may not have been identified. In contrast, the tourniquets placed in TFC are placed more deliberately after uniform/clothing has been removed and 2-3 inches above the identified site of bleeding.
How long should direct pressure be applied onto packed hemostatic dressings?
3 minutes.
Why is it important to check the pulse after applying a pressure bandage?
A pressure bandage should not be a tourniquet. It is important to check to ensure a pulse is still present distally after bleeding has been controlled by application of a pressure bandage. If no pulse is present the pressure bandage should be loosened and reapplied.
What is inguinal junctional hemorrhage and how is it treated?
Inguinal junctional hemorrhage is bleeding from the large blood vessels at the junction where the lower extremities join the torso. Injuries to these junctional areas are typically not amenable to a limb tourniquet and require other intervention. If available a CoTCCC-recommended junctional tourniquet should be applied. If not available, the wound should be packed with hemostatic gauze and direct pressure applied to the wound. Application of an improvised pressure delivery device may be needed to apply additional, targeted, and sustained pressure to control hemorrhage.
Injectable hemostatic agent is contraindicated in which types of wounds?
This device is not indicated for use in thorax, pleural cavity, mediastinum, abdomen, retroperitoneal space, sacral space, above the inguinal ligament, and tissues above the clavicle