Interfacility Transport of Patients Between Theater Medical Treatment Facilities
Joint Trauma System
Interfacility Transport of Patients Between Theater Medical Treatment Facilities
INTRODUCTION
Reducing the time to required medical or surgical interventions prevents death in potentially survivable illness, injuries and wounds. When evacuation times are extended, en route care (ERC) capability must be adequately expanded to mitigate the delay. In January 2010, the Joint Force Health Protection Joint Patient Movement Report stated “the current success of the medical community is colored by the valiant ability to overcome deficiencies through “just-in-time workarounds;” many systemic shortfalls are resolved and become transparent to patient outcomes. However, future operations may not tolerate current deficiencies.”1 This Joint Trauma System (JTS) Clinical Practice Guideline (CPG) recommends the minimum requirements and capabilities for the movement of critical care patients between medical treatment facilities (MTFs). It is designed to mitigate historically recognized and potential future systemic shortfalls with the ultimate goal of improving case fatality rates, reducing morbidity, and eliminating preventable death. This guideline is also referred to as the inter-facility transport CPG for policy adoption within a Geographical Combatant Command (GCC) or Area of Operations (AOR). The focus of this guideline is to establish a system of systems approach to identify the clinical and operational elements essential to optimizing the ERC of patients during inter-facility transport across a combatant theater, to include austere and far forward locations. Transport may occur via land, sea, or air and involve multiple agencies or coalition partners.
Successful implementation of this CPG first requires medical personnel with the appropriate education, training and capabilities throughout the ERC system. Secondly, the use of specialized transport equipment, supplies, and protocols required to meet the clinical needs of patients in transit are detailed. Also, it cannot be over emphasized that success requires effective coordination between the medical team, vehicle operators and the command providing the vehicles. Care capability is almost always reduced during ERC. The tyranny of distance is related to time. Further complicating this threat with en route delays will contribute to preventable deaths. Effective communication, coordination and cooperation across the system mitigate this risk.
Through this CPG, the Committee on En Route Combat Casualty Care (CoERCCC) and the JTS strongly recommend the establishment of a positive, proactive and responsive medical direction capability along with dedicated medical dispatch centers to facilitate patient care and safety during the phases of transport. These phases consist of pre-movement (e.g., patient preparation and packaging), en route (e.g., continuation of care and management of acute complications), and post-movement (e.g., review of documentation and patient outcomes) overseen by direct and indirect medical leadership. A systems of systems approach will help mitigate the risks associated with patient transport, and as described in this CPG will include: expected ERC capabilities, types of ERC providers, transport platforms and medical materiel, dispatch centers, medical direction, treatment protocols, documentation of care requirements, and patient transfer criteria.1
Unity of command is critical in this endeavor. While “unity of effort” suggests that multiple parties are working toward a shared goal in a coordinated way, it is not the same as “unity of command.” Unity of command represents a unified and focused effort that is essential for success in complex objectives. Specifically, “unity of command” is predicated on one person ultimately being in charge of the process though many people are working toward the outcome.2 Commanders must establish leadership positions with defined roles, responsibilities and the delegated authority to execute successful ERC. Competent military authority of the ERC system is required because success involves the synchronization of multiple teams, the transfer of patient care across those teams, and the myriad challenges of delivering care in operational environments. Subsequently, capability requirements for ERC must be established, promulgated and effectively enforced to ensure that the capability to deliver life-saving ERC is afforded the ill, injured and wounded.
This guideline is specifically concerned with the inter-facility transport of patients between the intra-theater roles of care including transfer between MTFs and civilian treatment facilities. Please refer to Tactical Combat Casualty Care-Tactical Evacuation Care guidelines for Point of Injury (POI) transport and to Aeromedical Evacuation (AE) guidelines for inter-theater transport.
It is important to note, in an immature theater of operations or in a larger scale conflict, casualty numbers may exceed available resources. When this occurs, compliance with this guideline may be compromised. Commanders need to ensure appropriate patient movement resources are a priority, especially for critical care transports between treatment facilities.
BACKGROUND
After years of conflict in Iraq and Afghanistan, the Military Health System is rightly proud of a 98% casualty survival rate for patients reaching a Role 3 facility. Unfortunately, this statistic excludes those casualties who die before reaching the Role 3 facility. According to Eastridge et al in Death on the battlefield (2001–2011): Implications for the future of combat casualty care, 87.3% of the total combat deaths occur prior to arrival at the Role 3 facility, highlighting the opportunity for further improvements.3 ERC is a significant patient care component both from the POI to an MTF and after damage control resuscitation and surgery to the next MTF or to an aerial port of debarkation (APO) for movement out of theater.
Inter-facility transport presents an "added challenge" and is associated with increased risk to the patient.4,5 These movements typically occur in combatant vehicles and, due to physical space limitations and operational demands, there are fewer providers giving care. And, while the number and complexity of interventions are limited, they are also more difficult to execute. Noise, vibration, and cramped spaces act together to disconnect lines, displace tubes, shift dressings, impede patient monitoring, and directly antagonize injuries. Environmental conditions and inclement weather during transport can contribute to morbidity and mortality. If flying, the reduced barometric pressure results in lowered partial pressure of oxygen, increased size of gas pockets, decreased tissue perfusion, and increased tissue swelling.6 The enemy and diplomatic considerations may also effect routes, duration of transport and the safety of movement. Good ERC systems and teams recognize these risks and mitigate their threats.
Transporting patients is a medical intervention itself and although very common still has risks and benefits. A central tenet of combat medicine is clearing the battlefield by transporting patients between facilities. Transport may be required because of the patient’s condition or the organization’s mission. The reality of war and military doctrine is that casualties must be evacuated until they receive definitive treatment. Consolidation and centralization of medical resources reduces their physical footprint, diminishes the need for re-location during combat maneuvers, avoids the loss of medical capability during re-location, and decreases the associated global logistical demands on the combatant command. The decision to transport is nearly reflexive, and rightly so. But, the risks inherent to transport must be minimized through a robust system of care dedicated to optimizing patient outcomes during transport. Besides the direct medical risk to the patient of the physical movement, loss of the transport asset and crew to accident or enemy action is real. There are many recurrent examples of both civilian and military medical evacuation helicopters being lost to environmental threats and enemy action flying missions that were probably not critical to life, limb or eyesight.
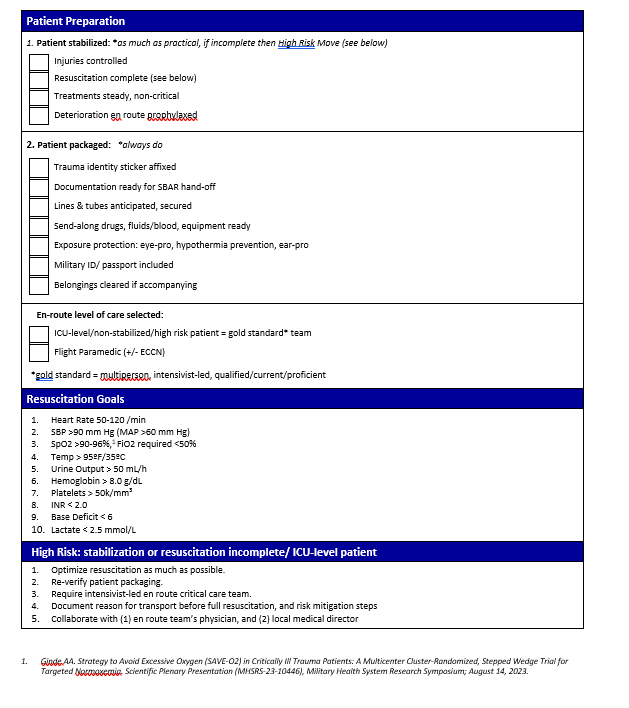
Patient Stabilization
In order to minimize transport contribution to morbidity and mortality, optimal but not necessarily definitive patient stabilization before transport is critical and encompasses four connected elements. First, injuries—actual and potential (e.g. spinal instability)—must be controlled. This usually happens at the earliest phase of tactical combat casualty care. Second, resuscitation must be optimized but may be ongoing. The best outcomes occur when a patient’s physiology is closest to normal before transport.7,8 Patient variables that best indicate adequate resuscitation for transport continues to be an area for continued basic and translational research.9,10,11,12 Third, other treatments besides resuscitative measures should be at steady-state, not requiring dynamic, complex, or life-preserving adjustments en route. Until technology progresses, the planned initiation of new interventions or the continuation of complex or capability unique interventions during transport are discouraged. Finally, deterioration requiring en route intervention must be anticipated and prevented with risk mitigation procedures prior to departure. Examples include placing lines or tubes, or decompressing compartment syndromes, as well as providing adequate analgesia for the increased pain of transport. This requires an understanding of the injury course as well as the transport environment.
Preparation for transport must include more than just patient physiology. Packaging to ensure safety during the transitions of care is also essential. This includes the logistical and the indirectly clinical aspects of getting the patient ready for transfer from the treatment facility to the ERC team. Many of these steps can be managed by the non-physician members of the transferring team but must be verified by the ERC providers prior to departure.
Expected ERC Capabilities
Medical capability is the quality or state of being able to provide the expected and required medical services and support to the casualty. Within the system of en route care, and when capability is discussed in this document, it is the ready and available potential to provide the required critical care in a proficient and timely manner. It includes the physical and mental talent of the team, as well as the physical presence of all medical materials and equipment in the vehicle that are expected by theater policy. A capability does not exist if the personnel are not proficient or if they are missing medical supplies and equipment. Nor is capability present if the ERC team is not integrated effectively with the transport platform team. Therefore, units must be conversant and compliant with the published theater standards along with being physically and materially ready to execute the assigned mission. Within the operational theater it is critical to ensure actual capability is effectively communicated between medical control, the transferring facility, the ERC team, and the receiving facility. The ERC organization has a moral, ethical and legal obligation to ensure they can carry out their mission essential task list and mission essential care capability for the patient. If not, they must notify their commander, the medical director, and the medical dispatch center that they are unable to provide the expected and required care to our critically ill, injured or wounded patients. Since medical evacuation is a theater asset, the local unit commander cannot legitimately accept risk for the theater commander. Locally accepting risk of a reduced capability compromises care, contributes to excess morbidity and mortality and is inconsistent with the effective and efficient use of medical dispatch centers. It is the center’s mission to select and assign the appropriate evacuation asset to the right mission.
A minimum of two levels of capability are recognized in this guideline: Critical Care and Intermediate Care. The ideal military ERC system will be a scalable and modular asset with appropriate resource allocation to provide a full range of patient care services to include advanced clinical capabilities.
Critical Care transport is required when “the patient has a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient's condition during transport.” For success, en route critical care must be provided by a team of providers “with the requisite decision making skills of high complexity to assess, manipulate, and support vital organ system failure and/or to prevent further life threatening deterioration of the patient's condition during transport.”13 Ideally, this team will be led by a physician or other independent practitioner with extensive critical care experience and the requisite equipment to perform lifesaving interventions as required by the clinical scenario.
Sometimes a completely packaged and fully stabilized patient is operationally unrealistic. Some injuries or illnesses cannot be stabilized due to capability limitations. Limited capability may be the driving indication for transport. These transfers are fraught with the risks of undesired outcomes during transport. Subsequently, the transferring provider should document the indications for transport before patient movement, continue the resuscitation and ensure adequate (even higher) capability of the ERC. The gold standard for unstable patient transport is movement with critical care capability led by a physician who is qualified, experienced, and proficient at critical care transport.
Intermediate ERC should be initiated for a patient that does not require critical care but is in need of a dedicated medical attendant with at least the knowledge and skills equivalent to a paramedic as defined by the National Emergency Medical Services (EMS) Scope of Practice Model. Adequate medical supplies to perform lifesaving interventions as well as ongoing resuscitation are also necessary. Patients in this category have some complexity of care delivery that must be maintained by a medically skilled provider but are not expected to deteriorate during the period of the patient movement.
Required ERC capability should be based on the current condition of the patient being transferred and their expected course during transport. This is determined by the transferring provider. If the requested level of ERC is not available, then a higher level of care should be provided. If this is not an option, then the transferring provider and the operational commander must carefully weigh the risks of patient transfer using a lower capability versus the risks of transport delay.
Commanders
Types of ERC Providers
Health care teams are comprised of a variety of different provider types, and the ERC mission is no exception. ERC providers must receive formal education and training to ensure platform familiarization and vehicle crew resource management. Updating military ERC systems based on cautious application of civilian best practices should be tempered by a realistic understanding of operational considerations. Over 67% of civilian Helicopter Emergency Medical Services (HEMS) agencies in the United States staff their helicopters with Critical Care Flight Nurse/Critical Care Flight Paramedic teams.14 Most ground EMS agencies use some variation of an Emergency Medical Technician (EMT) and Paramedic team. International HEMS agencies frequently use physician-led critical care transport teams.
The National EMS Scope of Practice Model is the core document that describes scope of practice for civilian EMS providers in the United States. These civilian levels of EMS provider, typically applied to enlisted medical providers, are Emergency Medical Responder, EMT, Advanced EMT, and Paramedic. Registered Nurses with education and training applicable to prehospital care have several advanced certifications available to validate their skill and knowledge proficiency, to include: Critical Care Flight Nurse, Certification in Emergency Nursing, Critical Care Registered Nurse, and others. Although not common in the United States, several international EMS systems educate, train, and certify physicians as prehospital providers and the United Kingdom (UK) Medical Emergency Response Team (MERT) platform is the most well-known from use in the Regional Command South of Afghanistan.
Higher competency and capability improves case fatality rates when patients are transported. During Operation Enduring Freedom, care provided by critical care flight paramedics showed a 66% lower risk of 48-hour mortality compared with that of basic level EMTs.15 In the UK, prehospital critical care is provided by physician-staffed HEMS. These teams have demonstrated survival in cases previously thought to be non-survivable (e.g., traumatic cardiac arrest).16 British military platforms with on board intensivists have likewise demonstrated improved survival in more severely injured patients.17
It is imperative to understand the attributes of the different provider types based on their qualifications and certifications. Instrumental to ensuring capability is the verification of currency of their practice experience and their skill proficiency. Additionally, well trained teams improve outcomes so ERC teams who train together prior to operational assignment may optimize patient outcomes.
Transport Platforms and Medical Materiel
Patient transport is conducted as a planned component of a given mission aboard dedicated vehicles or transports of opportunity. Understanding the capabilities and limitations of the transport platform will help ERC providers, mission planners, and medical control optimize the care they deliver. This requires the appropriate selection capability to conduct the mission based on the provider team, resuscitative equipment, treatment protocols and vehicular capabilities to move through the environment. For some ERC missions, the transport may require serial transfers between different vehicles and modes of transport. Familiarization with the different vehicles available in a theater of operations is imperative.
Weight and space restrictions, as well as the challenges of patient transport in an operational setting, necessitate the deliberate and careful selection of medical materials for a given mission. The provider’s competency and the medical material actually present in the vehicle determine ERC capability. Vehicle selection will directly impact personnel and equipment availability and determine the highest level of care. Vehicles should be chosen with an understanding of the patient condition and must be appropriate for the type of ERC provider. Specific medical materials designated as patient movement items (PMI) must be available to support the patient during every phase of transport. Examples of PMI include ventilators, patient monitors, pulse oximeters, suction machines, IV pumps, oversized litters, negative pressure wound vacuums, pneumatic compression stockings/devices and more.18 It is important the transferring facility request these items so that they can be loaded and transported with the ERC team. Whenever possible, the expendable medical supplies like oxygen from the transferring facility should be used until the last safe moment before departure. This action conserves the onboard medical supplies which cannot be replenished without stopping and delaying the transport. Additional information on PMI is found in the Aeromedical Evacuation Equipment Standards (AFI 10-2909), JP 4-02 and FM 4-02.1.
Dispatch Centers
Tasking of limited resources while providing an appropriate ERC response requires a dedicated team with a comprehensive and current understanding of its assets and their current capabilities. This dispatch center should allocate resources based on mission requirements, the request of the transferring provider, the expected need from across the catchment area, and the capabilities of the available ERC units. Medical evacuation dispatch centers can vary but all should be co-located within a command and control (C2) communications center to coordinate efforts. Examples of dispatch centers include the U.S. Army’s Theater Patient Movement Center for ground and rotary air ambulance medical evacuation and the joint activity Patient Movement Requirements Center for fixed wing aeromedical evacuation assets. Some multi-national AORs have Patient Evacuation Coordination Cells as dispatch centers for medical evacuation.19,20,21 Whatever the configuration of the dispatch center, they require detailed information to ensure the best allocation of available resources. This detailed information includes the validation and the verification of capability as resources increase and decrease with operational tempo and demands.
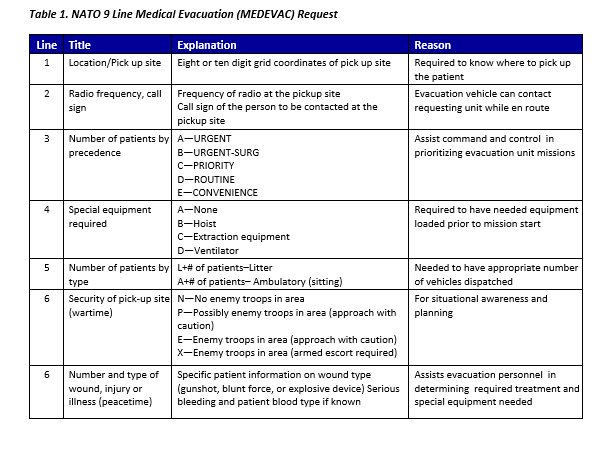
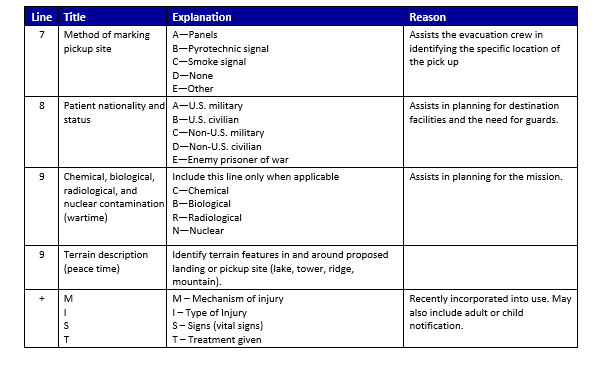
The 9-line medical evacuation request provides critical decision-making information in a standardized message format that helps expedite the medical evacuation process. A patient’s condition, the operational situation, terrain, weather conditions, enemy threat and availability of assets are communicated in the 9-line request and taken into consideration by the dispatch center when determining the best transport vehicle and type of provider to send. Accurate medical evacuation precedence determination ensures an appropriate dispatch of capability. Urgency of medical care provided by the transferring facility is used to determine the medical evacuation precedence. The senior military person (or designated on-ground mission commander) present in coordination with the senior medical person determines when to request medical evacuation and the precedence assigned to the patient for evacuation. The on-site personnel should determine the evacuation precedence and discrepancies between the ground force precedence and the dispatch center will err on the side of higher acuity with further discussion reserved for after mission completion and the immediate run review process.
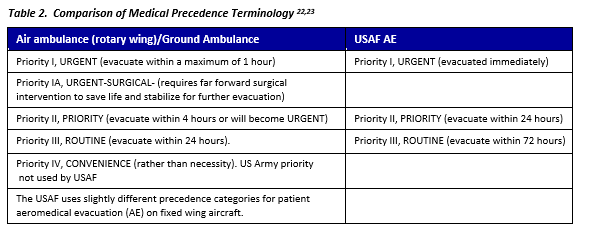
CAUTION: Terminology used to communicate precedence is not consistent across services. Terminology for air (rotary wing) and ground ambulances shall be used for inter-facility transports and is provided in Table 2.
Medical Direction
Medical direction is a critically important aspect of ensuring the delivery of an expected capability of care in the out of hospital environment.24,25,26 While medical direction may be delegated to any physician regardless of specialty, it does require some unique knowledge and skills. Medical direction has traditionally been the responsibility of the unit physician (flight surgeon for example), although most of these providers do not receive additional formalized or structured education or training for this duty.
Medical direction encompasses both online and offline clinical guidance.24 This CPG defines medical direction as the direct technical authority to determine capability, promulgate medical policy, and most importantly, the authority to enforce the standard of care through quality assurance with local privileging (official designation of ability to perform medical mission not necessarily the hospital version of “credentialing”) actions of individual ERC providers. Online medical direction includes both the on-scene medical supervision of providers actively engaged in patient care, as well as real time clinical guidance of providers via telecommunication.27 Offline medical direction includes protocol development and review, continuing education of prehospital providers, quality improvement activities, and other duties designed to increase the quality of the system but are not related to immediate and direct patient care.24 Medical direction can occur at many levels. This CPG will focus on the requirements and responsibilities for unit level medical direction and regional medical direction. The primary mission of the medical director is to ensure the commander is effectively advised on the technical requirements of medical evacuation and the transport unit is meeting expected patient care capability and quality.
The commander of the unit assigned to perform medical evacuation should appoint the unit’s physician as the medical director. The medical director is responsible for the technical control and supervision of all en route medical activities of the command and should be delegated that authority in writing. This additional duty order should also include the authority to privilege ERC providers within that organization. It should also include delegation of the authority and prerogative to hold in abeyance, to deny, or to immediately but temporarily suspend clinical privileges/practice when there is reasonable cause to doubt the individual’s competence to practice or for any other cause affecting the safety of patients or others. The specific intent of the medical director’s decision to implement temporary adverse privileging actions should be the safety and well-being of all patients and safeguarding the quality and efficiency of care delivered by the ERC organization. If a unit physician is not available to provide medical direction the unit conducting medical evacuation should coordinate with the supporting medical treatment facility for a shared medical director.
Minimum RECOMMENDED Qualifications (UNIT MEDICAL DIRECTOR)
- Duly commissioned officer in the Medical Corps of the Armed Forces of the United States.
- Knowledge of ERC mission provided by the unit, unit treatment protocols and CPGs, and capabilities of unit’s providers.
- Completion of the Tactical Combat Medical Care or similar course.
- Completion of the Joint En Route Care Course (if rotary wing unit) or similar course.
- Medical director and operational medicine training.
Desirable Qualifications (UNIT MEDICAL DIRECTOR)
- Board certification or eligibility in any specialty recognized by American Board of Medical Specialties or American Osteopathic Association or experience in operational medicine.
- Previous operational medicine assignments.
- Experience in medical direction for ERC.
Responsibilities (UNIT MEDICAL DIRECTOR)
Offline medical direction:
- Chart reviews of all cases personally or through delegation.
- Continuous quality improvement/practice improvement activities.
- Detailed case reviews on selected cases from chart review protocol variations or high risk low frequency interventions.
- Protocol development.
- Develops criteria for types of providers needed to transport patients based on clinical condition.
- Oversight of education and training of unit medical providers.
- Notify the next higher level of command surgeon/theater medical director of systemic issues identified.
- Conduct a quality assurance program and performance improvement program to ensure standardization of care delivered in accordance with regulations or instructions and Service and Combatant Command policies while validating practices and to propose new practices in ERC.
- Unit privileging, through technical oversight and supervision, ensuring that providers are qualified, current and proficient in their ERC duties and responsibilities.
- Ensures completion and delivery of patient care reports into the patient record and the Joint Trauma System.
Online medical direction:
- Due to communication and patient care challenges unique to the deployed environment online medical direction may be most effectively done by physicians other than the transporting unit medical director.27
- Priority of online medical direction is:
- Transferring physician.
- Receiving physician.
- Transporting unit medical director.
- Transporting unit medical director is responsible for ensuring providers know who and under what circumstances to call for online medical direction. It is important to plan/discuss whenever possible any anticipated scenarios requiring deviation from established ERC provider protocols with transferring physician to ensure required medical supplies are available during transport.
Medical direction is required at the unit level and also at the regional level (Patient Evacuation Control Center). Medical direction at the regional level is centered on offline medical direction activities. Regional medical direction works continuously to increase the quality of care delivered during intra-theater transport. Regional medical direction may occur at different levels based on the operating environment but will typically be at the level of the joint operations area and lower. The Joint Force Surgeon’s office is the doctrinal proponent for intra-theater patient transport and should assign regional medical directors. A best practice is to appoint a consultant at the Combined Joint Task Force level for EMS and ERC. The Joint Force Surgeon’s office shall provide regional medical direction unless they delegate this authority to subordinate regional medical directors.
MINIMUM QUALIFICATIONS (REGIONAL MEDICAL DIRECTOR)
- Board Certification in a specialty recognized by the American Board of Medical Specialties or American Osteopathic Association, and experience in Operational Medicine and/or extensive experience in en route care.
- Knowledge about the transporting environment and capabilities of units operating in theater.
Desirable QualificationS (REGIONAL MEDICAL DIRECTOR)
- Previous work as a unit medical provider.
- Board eligible/certified in EMS (vice fellowship training in EMS).
Responsibilities (REGIONAL MEDICAL DIRECTOR)
- In conjunction with medical planners advise the Combatant/Theater Commander on medical common operating picture and allocation of resources for intra-theater transport.
- Ensure requirements of documentation of intra-theater transport care are done.
- Assist medical directors operating in theater and ensure that they have the knowledge and skills to perform the job.
- Provide technical supervision to medical directors in theater.
- Ensure relevant out of hospital research is supported and accomplished.
- Ensure information from intra-theater transportation is supplied to the DoD Trauma Registry.
The Committee on En Route Combat Casualty Care of the JTS recommends the development of service-agnostic courses for Medical Corps officers to serve as entry level training for Medical Directors covering the fundamentals for physician leadership in EMS and ERC oversight and direction.
Treatment Protocols
The recognition of the importance of hospital based CPGs prompted the Institute of Medicine to release a report in 2006 recommending the development of an “evidence-based model for pre-hospital care protocol for the treatment, triage, and transport of patients.”28 By using a consistent approach to a particular kind of patient, it is hoped that critical actions will not be missed, less overall errors will occur, and the patient will get the appropriate, evidence based treatment required. A prehospital medical protocol is directive in nature and guides non-physician providers with patient care decisions in the absence of on-scene or online physician direction. Given their limited scope of practice, the providers are generally expected to follow the protocols as written. The use of protocols is already wide spread throughout the civilian ground and air medical transport arena, as well as within the U.S. Army’s new critical care flight paramedic program.
A systematic review looking at the effect of evidence-based clinical guidelines on patient outcomes in the Netherlands found that there was a significant improvement in the process and structure of patient care, and a smaller but significant improvement in outcomes.29 Another retrospective study reviewed patient outcomes after the implementation of a series of evidence based protocols in an intensive care unit. They noted a small but significant decrease in mortality after the protocols were instituted.30 A pre-hospital related study compared on-line medical direction of EMS personnel by an emergency nurse to a protocol based method of medical direction. The study found that there was a small improvement in the appropriateness of treatment decisions and a decrease in on scene time in the protocol based group as compared to the online group.31
While there is a limited amount of system based protocol research, there are many examples where the implementation of individual protocols have improved patient outcomes.32,33
In addition to guiding patient care, protocols also provide a means for performing quality assurance and developing research.34 By providing a standardized approach to medical care, any deviations from the protocol can be noted, evaluated, and addressed as needed across the EMS system. When gaps in practice are identified, there is also potential for research into causes and solutions to address them. These protocols require regular review and at minimum annual revision.
Documentation of Care
- Inter-facility patient transports must be documented on an approved patient care record (PCR).
- JTS approved PCR’s include:
- DD Form 1380 Tactical Combat Casualty Care (TCCC) Care
- DA 4700 overprint Tactical Evacuation Patient Care Record (JTS approved 20141119)
- AF IMT 3899 Patient Movement Record (20060819, V1)
- Medical Rescue Report SAR Form 3-50.1A
The Tactical Evacuation Patient Care Record is primarily used for rotary wing transports from point of injury or inter-facility transfer. The AF IMT 3899 is primarily used for Aeromedical Evacuation, with supplements A through K as indicated for Critical Care Air Transport Team movements. The Medical Rescue Report SAR Form 3-50.1A is required whenever a search or rescue is attempted or accomplished that involves Navy personnel or assets. (NTTP 3-50.1)
When completing the PCR, it is important to ensure that the patient’s name on the PCR matches the name entered on arrival to the MTF. In cases where a casualty’s name is unknown, the MTF will utilize theater predetermined trauma identities. Transport teams must obtain an ID sticker at the time of handover to the MTF to ensure the correct identity is recorded on the PCR.
The PCR should be completed and delivered to the receiving MTF along with the patient. Completed PCR’s and After Action Reviews may be submitted to JTS Prehospital at the following email address: usarmy.jbsa.medcom-aisr.list.jts-prehospital@mail.mil
At the time of handover to the MTF, the ERC team will provide a MIST (Mechanism, Injuries, Vital Signs, and Treatments) report summarizing the care received. The MIST report will be recorded by the receiving team on the DD Form 3019 Resuscitation Record for trauma patients, or in the Emergency Department record for non-trauma patients.
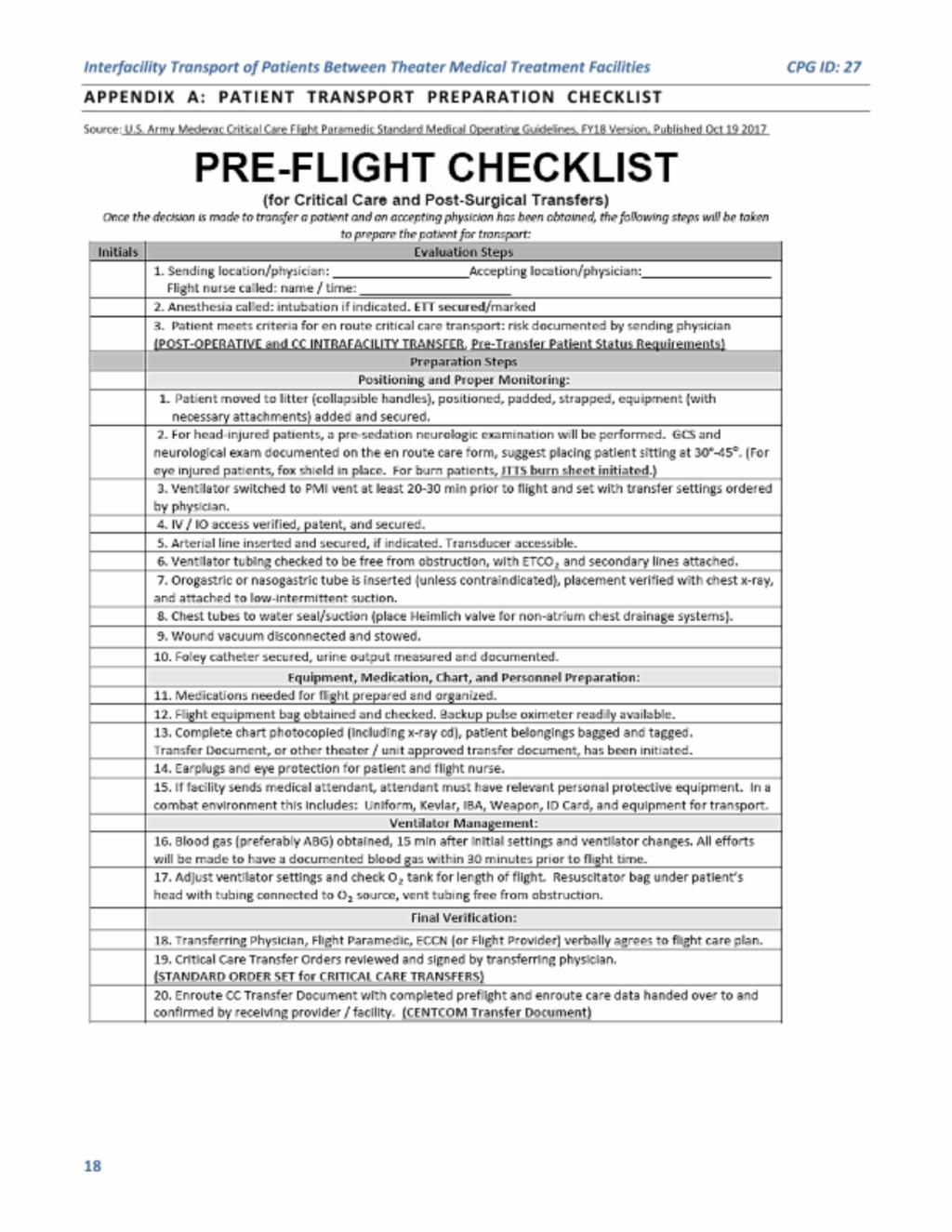
The CoERCCC and JTS recommend the development and implementation of ERC checklists for all phases of ERC that serve as clinical decision support tools. An example is found in Appendix A.
Patient Transport Criteria
Performance Improvement (PI) Monitoring
All transported patients (intratheater, interfacility within theater).
- All patients in population of interest have patient care documented on an approved record form.
- Casualties requiring mechanical ventilation are transported by an enroute critical care provider (critical care flight paramedic, enroute critical care nurse, critical care physician assistant, or critical care physician).
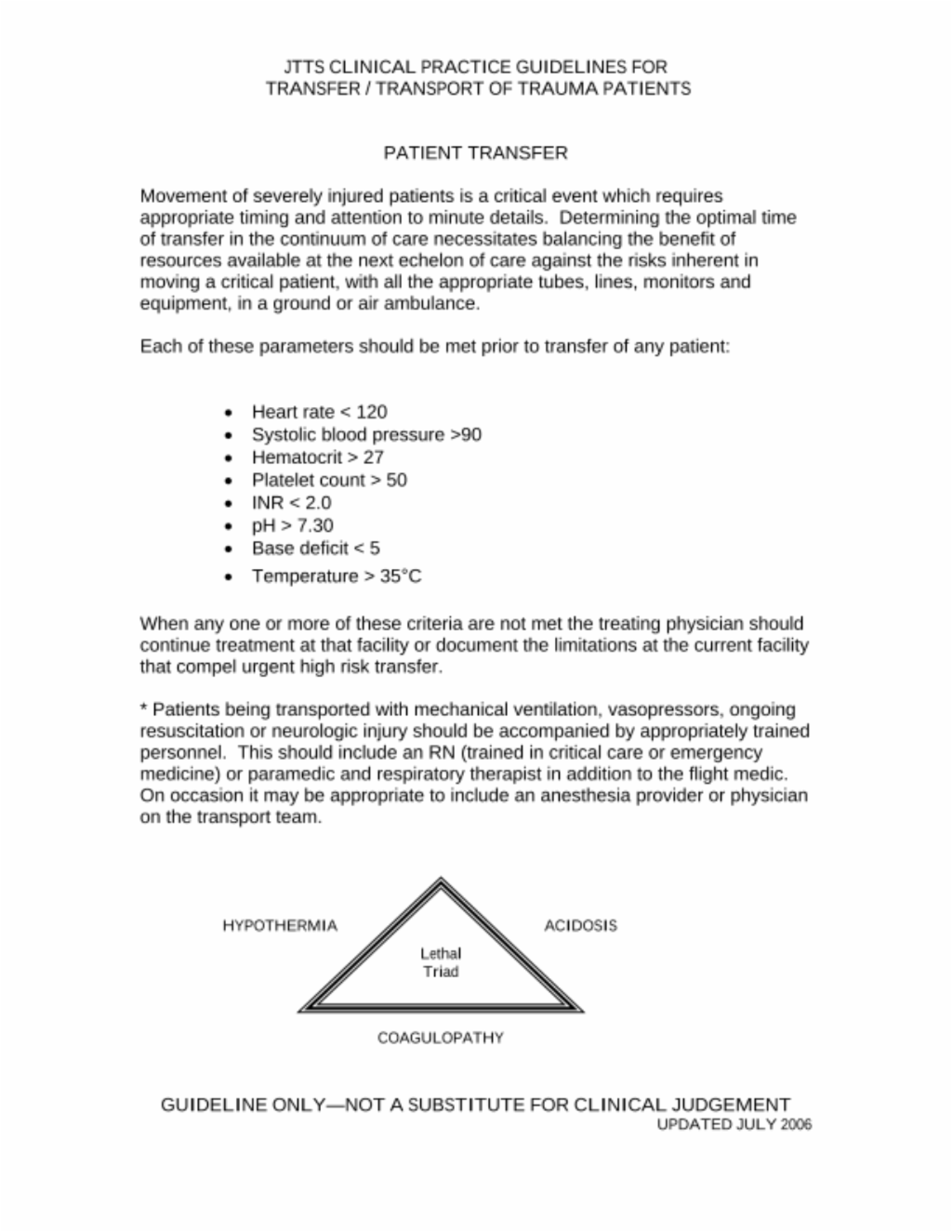
- Casualties are assessed for adequacy of resuscitation prior to interfacility transfer. For patients with any of the following parameters: HR < 50 or >120, systolic BP <90, core temperature <35 ℃, SpO2 <90%36 on supplemental O2, Hct <21, base deficit below -5, or pH < 7.3, documentation indicates the need for transfer prior to restoration of physiology to more normal parameters.
- Ventilated patients are placed on the transport ventilator, all monitors in place and stabilized for 30 minutes prior to departure from the current role of care to the aircraft and a final check for stability is performed/documented prior to wheels up and departure from that role of care.
- Ventilated patients will receive lung protective ventilator settings (e.g., tidal volume 6-8 ml/kg) and have ventilator settings documented.
- A hard copy of the medical record accompanies the patient.
Performance / Adherence Metrics
- Number and percentage of patients in the population of interest with patient care documented on an approved record form.
- Number and percentage of patients on mechanical ventilation who are transported by an enroute critical care provider (critical care flight paramedic, en route critical care nurse, critical care physician assistant, or critical care physician).
- Number and percentage of patients in the population of interest who are transported prior to physiologic stabilization (HR < 50 or >120, systolic BP <90, core temperature <35 ℃, SpO2 <90% on supplemental O2, Hct <21, base deficit below -5, or pH < 7.3).
- Number and percentage of patients on mechanical ventilation who are placed on the transport ventilator, all monitors in place and stabilized for 30 minutes prior to departure from the current role of care to the aircraft.
- Number and percentage of patients who had a final check for stability performed/documented prior to wheels up and departure from that role of care.
- Number and percentage of patients on mechanical ventilation who had ventilator settings documented.
- Number and percentage of patients on mechanical ventilation who had ventilator settings documented and with tidal volume 6-8 mL/kg.
- Number and percentage of patients who had a hard copy of the medical record that accompanied the patient during interfacility transfer.
- Patient Record
- Department of Defense Trauma Registry
The above constitutes the minimum criteria for PI monitoring of this CPG. System reporting will be performed annually; additional PI monitoring and system reporting may be performed as needed.
The system review and data analysis will be performed by the JTS Chief and the JTS PI Branch.
References
Appendix B: Additional Information Regarding Off-Label Uses in CPGs
Purpose
The purpose of this Appendix is to ensure an understanding of DoD policy and practice regarding inclusion in CPGs of “off-label” uses of U.S. Food and Drug Administration (FDA)–approved products. This applies to off-label uses with patients who are armed forces members.
Background
Unapproved (i.e., “off-label”) uses of FDA-approved products are extremely common in American medicine and are usually not subject to any special regulations. However, under Federal law, in some circumstances, unapproved uses of approved drugs are subject to FDA regulations governing “investigational new drugs.” These circumstances include such uses as part of clinical trials, and in the military context, command required, unapproved uses. Some command requested unapproved uses may also be subject to special regulations.
Additional Information Regarding Off-Label Uses in CPGs
The inclusion in CPGs of off-label uses is not a clinical trial, nor is it a command request or requirement. Further, it does not imply that the Military Health System requires that use by DoD health care practitioners or considers it to be the “standard of care.” Rather, the inclusion in CPGs of off-label uses is to inform the clinical judgment of the responsible health care practitioner by providing information regarding potential risks and benefits of treatment alternatives. The decision is for the clinical judgment of the responsible health care practitioner within the practitioner-patient relationship.
Additional Procedures
Balanced Discussion
Consistent with this purpose, CPG discussions of off-label uses specifically state that they are uses not approved by the FDA. Further, such discussions are balanced in the presentation of appropriate clinical study data, including any such data that suggest caution in the use of the product and specifically including any FDA-issued warnings.
Quality Assurance Monitoring
With respect to such off-label uses, DoD procedure is to maintain a regular system of quality assurance monitoring of outcomes and known potential adverse events. For this reason, the importance of accurate clinical records is underscored.
Information to Patients
Good clinical practice includes the provision of appropriate information to patients. Each CPG discussing an unusual off-label use will address the issue of information to patients. When practicable, consideration will be given to including in an appendix an appropriate information sheet for distribution to patients, whether before or after use of the product. Information to patients should address in plain language: a) that the use is not approved by the FDA; b) the reasons why a DoD health care practitioner would decide to use the product for this purpose; and c) the potential risks associated with such use.
Download CPG in PDF
READ FULL PDF
READ FULL PDF
READ FULL PDF
READ FULL PDF